The app is an innovative and evidence-based diagnostic tool that uses analytics to help clinicians understand the risk of pre-term labour more accurately. This improves the lives of women and babies by identifying those who truly need medical intervention and reassuring those who don’t.
The app was tested across 20 UK sites and the QUiPP Toolkit has now been recommended both locally and nationally by NHS England and the British Association of Perinatal Medicine.
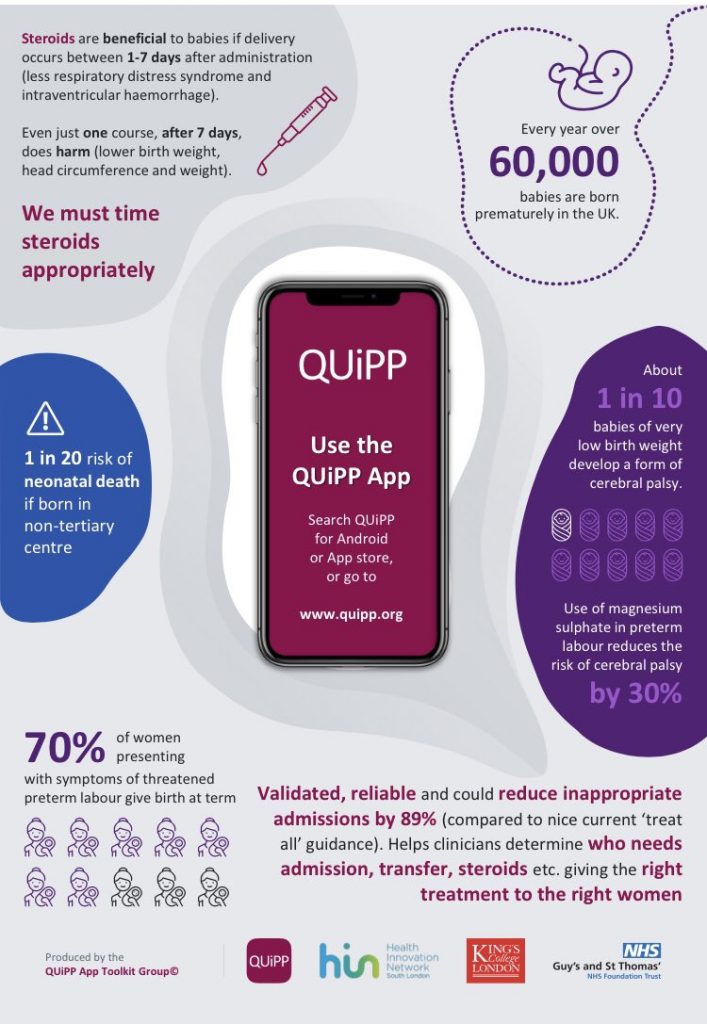
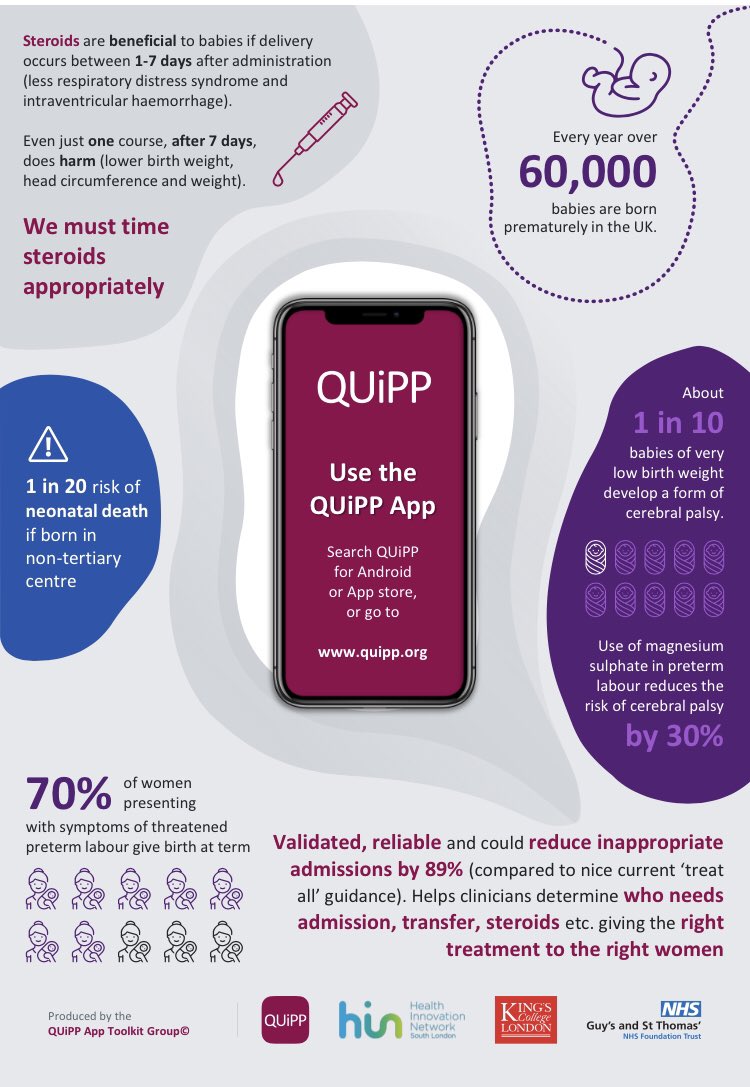
Pre-term labour is a clinical conundrum: it’s very common for women to be at-risk of pre-term labour, but the actual number of women who go on to deliver early is very low. To be safe, this means that many women are currently over-managed: they are treated as though they will deliver early even if the risk is low in reality. Because it is very dangerous to move an early baby once it is delivered, women at risk of pre-term labour are often moved to specialist hospitals further from home with specialist cots for early babies and are given more invasive care.
This tool has the potential to make a big difference and to improve care for these women. Whereas currently women are simply either ‘high’ or ‘low’ risk, the app calculates a percentage score so that clinicians can understand risk to a much higher degree of accuracy. This reduces the need for women at lower risk to move far from home and frees up the cots for the women who genuinely need them, so that people receive the care that is most appropriate to their risk and are not moved from their family and familiar midwife team if it is not necessary.
How does it work?
It’s a clinical decision support tool based on a validated algorithm that incorporates existing point-of-care tests and risk factors. A clinician enters information about a number of biomarkers, such as the scan that measures the cervical length and the swab on quantitative fetal fibronectin. QUiPP uses all the data across risk range for each variable and provides a user-friendly clinical interface. This is more useful for making management decisions and women find it very useful to see and discuss their risk as a percentage, with a highly visual aid to support discussions and decisions around treatment. The QUiPP app is free and has significant cost-savings associated with reducing unnecessary admissions and interventions. By freeing up NHS capacity for patients in the most need of care (eg maternal beds, neonatal cots), this intervention can save money and transform maternity pathways beyond the preterm birth setting. Qualitative findings suggest that the majority of clinicians involved in triaging threatened preterm labour found using the QUiPP app time-saving, simple and that it increased confidence in decision-making.
Professor Andrew Shennan, Professor of Obstetrics at King’s College London and Guy’s and St Thomas’ NHS Foundation Trust, said:
“This is a great example of the way that technology doesn’t replace clinicians, it makes our lives easier and helps us to care more effectively for our patients. QUiPP calculates the risk in a quick and visual way, giving women reassurance at a worrying time in their lives. What you really want is an exact chance of what’s going to happen. That way women and clinicians can make the most informed choices.
“These kinds of real-world testing are so important for scaling innovation. We hope that through this work, we can show the value of a tool like this and support others to use it in their practice.”
We also spoke to Naomi Carlile about the project one year on…
Tell us what has happened since the Innovation Grants:
I recently co-develop a toolkit to enable hospital sites across England to implement a best care pathway (the QUiPP Toolkit) for women who arrive in threatened preterm labour. I am now working on my NIHR Clinical Doctoral Fellowship, which is looking at how the Preterm Birth Surveillance Pathway is implemented across England (the IMPART study).
What has been your proudest moment so far:
I am proud that our QUiPP Toolkit has now been recommended both locally and nationally (by NHS England and the British Association of Perinatal Medicine), ensuring that more mothers and babies are receiving optimum care.
What your advice for future innovators:
Your good idea is a good idea! Get in touch with organisations like HIN south London to help advise on how to get it off the ground!