Get in touch
Need support with planning and delivering change programmes? Our team can help.
Email usThe new government has put change at the top of their agenda for health and care. In this blog, our Chief Executive, Rishi-Das Gupta, suggests that to make the changes needed effectively and efficiently, we first need to shift our leadership style, moving from a top-down "one way is the right way" mentality to a more "Buddhist" approach. This ethos emphasises flexibility, allows for diverse paths to a common goal, and embraces the strengths of local systems.
In an era where the healthcare landscape is ever-evolving, the new government’s commitment to change is a glimmer of hope for the National Health Service (NHS). It’s no secret that the NHS is grappling with a multifaceted crisis, driven by an aging population with increasingly complex health needs coupled with a progressively fatigued workforce. There is a broad consensus that the solution lies in involving people and communities more deeply in their care and encouraging healthcare providers to innovate… but it continues to be hard to spread innovation, we’ll explore why below.
Clinicians tend to cherish autonomy and the ability to adapt their practice to the patient in front of them. Hence, there is a vast diversity in practice and organisation driven by the preferences of both care providers and patients. This diversity is at odds with a leadership style that mandates uniform changes. In October 2022, Malte Haring, Felix Freigang, Volker Amelung and Martin Gersch conducted a systematic review of 29 papers outlining the tensions in healthcare innovation. They mapped these on a single, wonderfully complex page, highlighting why change often leads to conflict. However, understanding and navigating these tensions is critical for effective transformation.
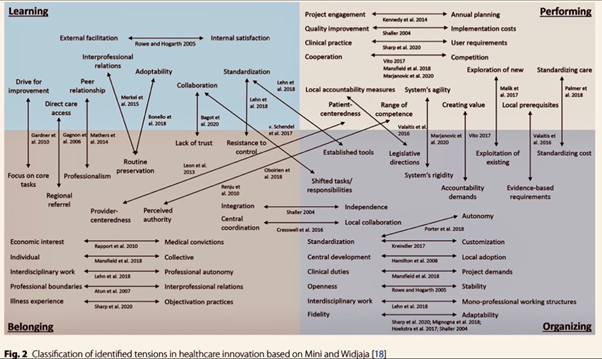
Figure 1: Classification of identified tensions in healthcare innovation based on Mini and Widjaja
The Stanford professors Bob Sutton and Huggy Rao, provide a simpler framework for this discussion (which I love) in their 2014 book “Scaling Up Excellence”. They describe two styles of transformation: the “Catholic” approach, characterised by a single, common method, perfected and then applied uniformly, and the “Buddhist” approach, which sets a defined endpoint but allows for multiple paths and paces to reach it. The NHS’s major change programmes have traditionally leaned towards the Catholic approach, aiming to mandate change and spread “best practices” uniformly. This approach, however, often overlooks the autonomy and diversity of service providers, leading to resistance and inconsistency in implementation.
The NHS is unusual in that the vast majority of care (around 90%) is provided by government-run organisations with similar values and employment practices. This leaves staff with relatively few options to work in healthcare outside the NHS and so creates resistance to change. Relatively small groups in a workforce can derail a change programme if they see it as a threat to their current preferred way of working, even if it is of benefit to other staff or patients. Furthermore, implementing significant changes in such a complex system usually requires lengthy public consultations which take a minimum of 14 months and are often costly.
To address these challenges, we need a shift in leadership style towards a more Buddhist approach. Policymakers must recognise that their ability to drive change is linked to incentives based on outcomes that matter to patients. Meaningful change does not need to be uniformly implemented; local systems should have the flexibility to tailor changes to their specific needs. The recent move towards Integrated Care Boards (ICBs) is a significant positive development in this direction. ICBs facilitate collaboration across health and care organisations, ensuring that local needs and circumstances are prioritised.
An example in south London has been the implementation of a national programme to improve medicines safety and reduce harm from prescribing opiates. Both ICBs in south London had identified reducing opiate use as a priority in advance of the national programme and worked with us at the Health Innovation Network to build a good understanding of what was needed for their systems.
South East London made extensive use of nationally developed approaches which focused on while South West London adapted the materials to reflect additional complexities in their local healthcare system. Both ICBs are now amongst the best nationally in terms of using opiates safely despite the differences in approach and have embedded this change locally through a sense of ownership by the local clinicians.
Additionally, developing varied, locally accountable innovation support structures like Health Innovation Networks is crucial. These networks provide the support and resources necessary to drive local innovation and improvement. Crucially HINs use implementation science. The implementation of lasting change or of spreading innovation across complex healthcare systems is a collective social process. In such complex adaptive systems negotiating the local context needs is crucial for implementation to be successful (this approach was outlined by my colleagues in a BMJ article (from 2020).
In conclusion, delivering change in healthcare can indeed be simple if our leadership embraces a more flexible approach. By allowing for diverse paths to a common goal and leveraging structures like Integrated Care Boards (ICBs) and developing locally tailored innovation support (including Health Innovation Networks), we can foster innovation and adaptability in our healthcare system. It’s time to move away from a one-size-fits-all mentality and towards a model that respects and harnesses the unique strengths of our healthcare providers and communities and empowers and supports them to change. Only then can we hope to build a resilient and responsive NHS capable of meeting the challenges of today and tomorrow.
Need support with planning and delivering change programmes? Our team can help.
Email us