Mapping of Bromley Virtual Ward Pathways
May 25, 2023
Background and context
Virtual wards allow people who need hospital care to receive the care they need at home, including in care homes, safely and conveniently rather than in a hospital. They provide systems with a significant opportunity to narrow the gap between demand and capacity for secondary care beds providing an alternative to admission and/or early discharge.
At the request of SEL ICB, The Health Innovation Network (HIN) gathered insights into the current state of the virtual wards in Bromley and highlighted current challenges, gaps, and opportunities.
More specifically, planned outputs were to:
- explore what improvements would support the delivery of the pathway
- produce a report highlighting key recommendations
- produce a process map representing the current pathway
This report details our approach and method as well as the insights and recommendations.
The Bromley virtual ward service
Virtual wards in South East London are led and coordinated by the community providers.
The One Bromley partnership has developed a hospital at home service to deliver a range of monitoring and interventions in the community that would otherwise be delivered in an acute hospital.
The service is provided borough-wide to people who need hospital care that are registered with a Bromley GP. Referrals are currently from the acute hospital, other urgent community response services and Bromleag, the GP practice for residents of nursing and care homes in Bromley. The service is a consultant-led multidisciplinary team currently consisting of GPs, consultants, nurses, and health care assistants with clinical accountability for its patients.
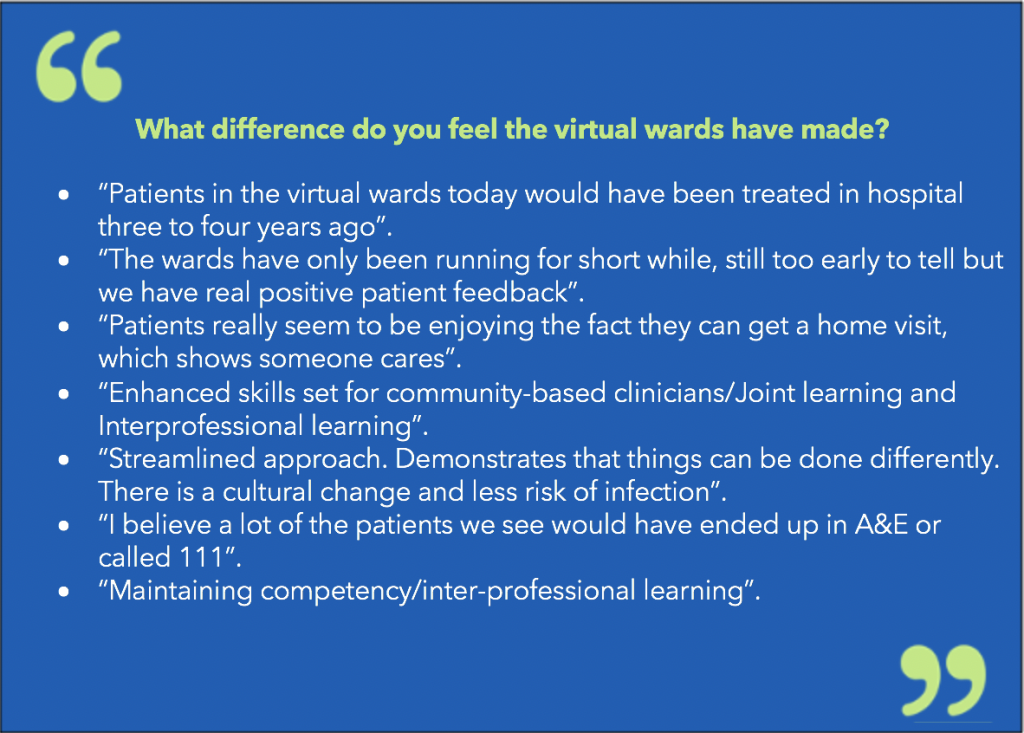
Findings
Findings indicated that effective communication and collaboration between healthcare professionals are critical for the success of virtual wards. The workshop participants identified the need to ensure continuity of care and effective management of available resources.
Additionally, the participants of the interviews and workshop emphasised the need for appropriate skill mix and more support of advanced clinicians to facilitate discharge.
Recommendations
Based on the insights from the project, several recommendations can be made to improve the virtual wards process and enhance patient outcomes. These include:
- Streamline the referral process
- Review data on the utilisation of the patient and staff telephone line
- Interoperability
- Multidisciplinary team meetings
- Review training, development, and skill mixing
- Patient information
- Review weekend escalation process
Recommendations from the co-design group
Following the workshops, the co-design group produced the below recommendations:
- Embed patient voice at governance level; invite people with lived experience to join sections of the board/steering group meetings which they can influence.
- Develop people-focussed outcomes for hospital at Home as well as clinical outcomes.
- Actively reach out to and engage people from ethnic minorities, non-English language speakers and people with additional communications needs to understand their experiences. These views were not captured via co-design workshops.
- Involve people with lived experience in staff training and development, invite people with lived experience to join training, offer training to informal carers and reverse mentoring for staff.
- Ensure all community staff, not just the Hospital at Home team, undertake deaf awareness and dementia training.
- Develop leaflets and advice on Hospital at Home in partnership with local people.
- Produce communications in accessible formats upfront so that all users are immediately catered for rather than retrospectively sharing things in accessible formats.
- Ensure all videos, technology and monitoring approaches are accessible to users with different needs.
- Join up with existing long term health condition services and care homes.
Conclusions
Overall, the virtual ward process mapping was a successful exercise that identified valuable insights and opportunities for improvement. The findings from the interviews and workshop will help to inform future strategies for improving the virtual ward process in Bromley, ensuring that patients receive the highest level of care possible. The project demonstrated the importance of collaboration and communication across teams, the complexities of meeting national and local ambitions to integrate services around the needs of patients, and the need for ongoing efforts to improve processes and systems to do this effectively.
