This module is designed to help eating disorders professionals understand:
• The life transitions taking place for many young people at the same time as transferring ED services• Pressures and practical considerations related to these changes
This module is designed to help eating disorders professionals understand:
• The life transitions taking place for many young people at the same time as transferring ED servicesIn a hurry? Use the buttons below to navigate through the content of this module.
Can you take a moment to think about some of the routes that people of this age may take and the pressures these might involve?
It is important to note that some of these transitions may be transient (e.g., university students returning home over the holidays).
This means that the young person and their families will have to navigate fluctuations in independence.
These transitions can be exciting but can also have a destabilising effect, even for young people who do not experience mental health difficulties.
It is therefore important for services to highlight potential difficulties associated with the move towards independence and support the young person to create tailored plans on managing independent living and when or who to seek help from.
“I thought recovery was going well, but I’d done absolutely no preparation … for mentally coping with the changes of moving to university. I think it was partly because of that that I became so much more unwell once I reached university.”Service User
Services should establish joint working practices with other institutions where possible. These can include local GPs, university mental health/wellbeing/sports services and local charities.
Some outreach ideas for service providers include:
Provide information to patients on services available before they move to university or in a different area and make sure you have up-to-date information on their new GP to be able to communicate effectively with them.
“I didn't know for sure where I'd be going to university, which was very soon after I turned 18 … that meant I didn't know which eating disorder service I'd go to cause it's linked to the city and I didn't want to stay with CAMHS and see yet another person from CAMHS.”Service User
Before you and the patient start planning a transition it might be helpful to think about whether now is the right time for them to be facing this.
In particular, you might find some of the below documents helpful in having discussions with the patient about this and making the best treatment plan for them:
Differences in referral protocol, provisioning, and commissioning between trusts can make it difficult to navigate accessing appropriate services when moving geographically; however, attempts should be made to avoid gaps in care:
As soon as you become aware of a possible transition, help the young person work towards a relapse prevention plan.
First, help them think about the difference between a lapse and a relapse.
A lapse represents a temporary slip or return to a previous behavior that one is trying to control or quit.
A relapse is when someone in recovery returns to disordered eating or weight control behaviours.
Other factors that might be helpful to consider include:
Whether patients are under or over eating, you can help them think about eating as being on a spectrum (some people are at the over-controlled end and some the under-controlled end) – the advice is meant to help them move towards the middle of the spectrum.
Help them plan a personal template for eating:
Download the FREED dietetics handout here with further information and tips for patients who might be struggling with chaotic eating/binge eating.
Help the young person think about how they will manage drugs and alcohol. It may also be useful to work through how they will approach new friendships, including setting boundaries or working through potentially sensitive conversations.
Make a plan to support the young person with eating out and eating with other people:
Top tips:
Help the young person think about how they will structure their time and support them in thinking about how they will balance work/studying, having a social life, self-care and leisure. For example, how will they manage exercise when at university or living independently?
Top tip:
Click the buttons below for some examples of what some service users suggested around structuring time:
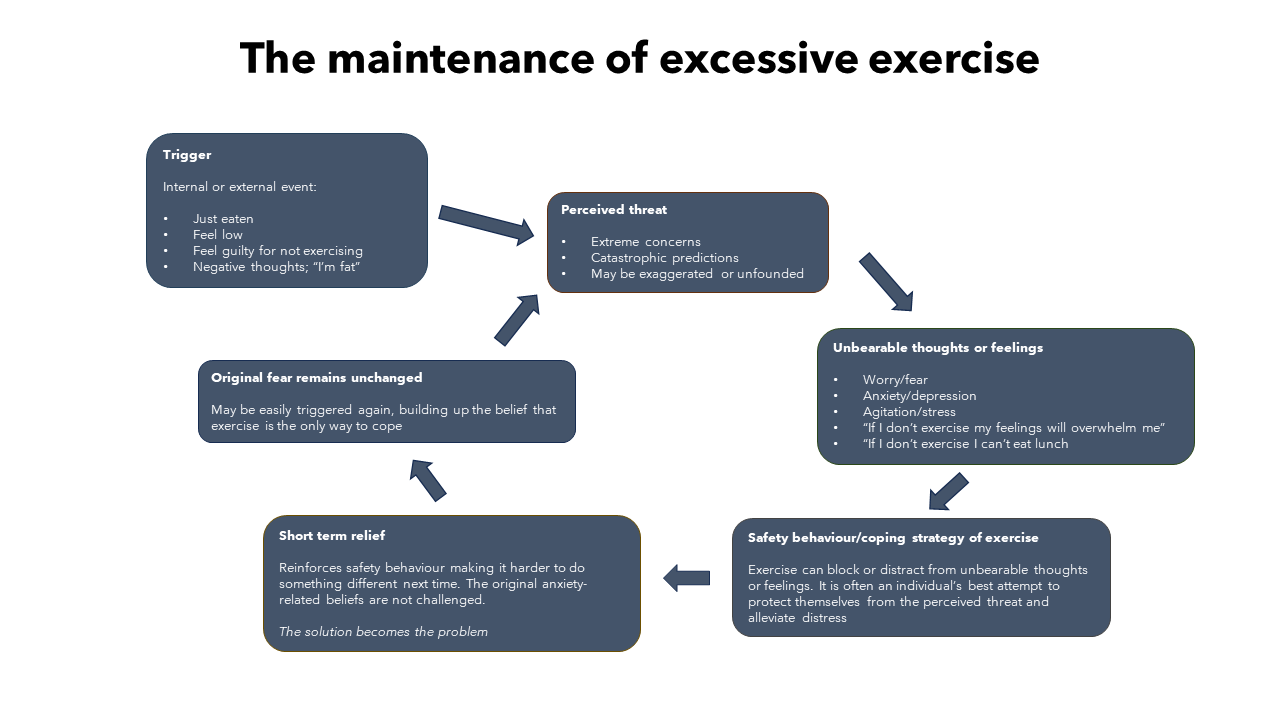
When thinking about transitions and in particular moving to University, it is important to address excessive exercise and how to manage this.
When preparing the young person to transition it might be helpful to think about exercise and how they are currently using it. If they are excessively exercising, it might be helpful to support them in recognizing when this is happening and what they can do to avoid this (particularly if joining gyms or clubs).
If helpful, help the young person create a personalised plan around exercise (how much each week) and, if planning to decrease it, create a plan on how they can do this in the upcoming weeks (e.g., keeping a diary and planning behavioural experiments).
You might find it helpful to use the diagram below to have a conversation about excessive exercise and think about ways of reducing this.
Start having conversations with the young person on whether it would be helpful for them to disclose their eating difficulties. Help them list the pros and cons of disclosing and of not disclosing.
Family dynamics and cultural/gender identity mean that the process of transition and emerging adulthood may be very different between individuals. It’s important to be open and curious about these differences, when talking about the transition process and in more general discussions as well.
Examples of individual circumstances and adaptations during a transition include:
Resources
Providing a space to think about the practicalities of independent living is important.
Problem-solving, providing practical resources, and practicing skills can provide patients with a realistic view of independence and increase a young person's confidence in their ability to cope.
Key practical areas to consider:
Resources:
Travelling abroad for work, study or leisure can present its own unique challenges for young people.
Different cultures can have varying attitudes and approaches to food.
Certain appliances (e.g., hobs and ovens) can be hard to come by while on the move.
Healthcare systems can vary widely in different countries.
Communication issues can arise from misunderstandings.
Travelling can often make people feel homesick or lonely.
Clinicians should encourage patients to consider their medical risks when deciding if moving abroad or travelling for a prolonged period is right for them.
Like any transition, specific, proactive planning on how to manage the experience itself as well as when/where to seek help is key.
There are several helpful resources on this topic you can refer to:
For many young people, going off to university is a rite of passage.
Moving out of the family home is often a natural part of this transition.While some may leave permanently, many young adults will return regularly, whether for weekends, term holidays or after graduating. However, for university students with eating disorders, this milestone presents a host of unique challenges. These challenges are not limited to the students themselves, as their families and caregivers may also face additional worries and concerns.
Download the Support for Carers Guide to learn more.
There is a thriving community of eating disorders professionals on FutureNHS. Click the button below to join and access support from fellow professionals.
Visit FutureNHS