This module is designed to help eating disorders professionals understand how to:
- Have conversations about transitions
- Establish a clear transition pathway
- Carry out person-centred planning
- Bring a transition to a conclusion
This module is designed to help eating disorders professionals understand how to:
In a hurry? Use the buttons below to navigate through the content of this module.
Most people agree on the cornerstones of person-centred transitions, with RCPsych guidance stating that transitions should be:
However, details on how to go about this in the context of an eating disorder are less readily available. In the video below, we hear from some young people and carers about what they felt worked well when it came to conversations about transitions:
We also spoke to experienced ED professionals about their advice about how to have conversations about transitions:
Listen to the clips below to hear from Esther, a Team Manager and CAEDS clinician for more than 20 years discuss how she might talk about transitioning from CAEDS.
1. Deciding when to have a conversation about transitions with young people
2. Transitioning in a motivational stance (particularly with newly-referred young people)
3. Opportunities for young people related to transitioning
4. Talking about transitions with families and the differences compared to discussions with young people
RCPsych Guidance states that services should have clear protocols and pathways for patients transitioning between them.
Based on work from the Worcestershire Health and Care NHS Trust Transitions Group, a joint CAEDS & AEDS transition policy may include:
As the young person moves through the transition pathway, it is important to keep track of their progress. Some suggestions for how to do this are shown below:
Maintain a database of useful patient information, including: Trust ID, date of referral, when they turn 18, current treatment status, status of transition, their last CAEDS session & “issues” log
Your team can meet weekly in 15 minute huddles to discuss patients under the CAEDS pathway. This ensures team members can delegate responsibilities, provide updates & receive support.
The clinician the young person is working with will help them to prepare for their transition & together they will work on a transition care plan. The co-ordinator will monitor the service user's care until they transition
RCPsych guidance also recommends having a well-structured, parient-centred care plan. But what does a patient-centred care plan actually mean?
We believe that it entails providing care that is tailored to suit the person's illness, situation and needs.
To this end, the plan should specify the following:
Models assessing preparedness and readiness to transition have been piloted with young people in physical health settings and, to a far lesser extent, in severe mental illness, but not (to our knowledge) in EDs.
One example of a model from physical health settings is the ReadySteadyGo transition programme, used by University Hospitals Southampton. This programme uses checklists to guide exploration of young people's confidence and skills in taking charge of their healthcare.
We can use the ReadySteadyGo transition programme to guide us towards some areas we might wish to explore for EDs:
Can you think of any other questions that might need asking?
RCPsych states that transition support should sensitively involve the family and carers. While many YP are happy for parents to remain involved in some capacity, others may want more autonomy when transitioning into AEDS.
In a low risk situation, you can discuss (and establish) with the YP their expectations around confidentiality & autonomy. Hover over the cards below to explore some questions and follow-up questions which could help to start conversations about confidentiality:
Can you imagine a scenario where we [AEDS team] are unable to reach you? E.g. your inbox is full, you’re overwhelmed with work, you’re feeling ambivalent about recovery.
Now imagine a higher risk situation, where the parents have been involved throughout CAEDS and the YP is ambivalent & only able to maintain therapeutic gains in outpatients because of parents' support.
In this scenario, you would want to be more ‘pushy’ about having contact with the parents. You might consider more direct lines of discussion:
"We need to have open channels of communication with your parents, otherwise it will be hard to work with you safely and support you in outpatients."
Once consent to contact is established, you can then negotiate what you would or would not tell the parents, including giving options.
Confidentiality is explored in more detail in Module 5 of this learning resource.
Click the buttons below to read about the different treatment stages of a CAEDS to AEDS transition for a low and high risk patient, along with reflective commentary.
Research suggests that phasing out CAEDS services may improve the transition process, by allowing the CAEDS team to follow-up with the YP after they have transitioned into AEDS (Nadarajah et al. 2021).
This should:
Can you think of additional adjustments to improve the post-transition process…?
Research by Broad et al (2017) found that young people also suggest a number of contributing factors for a positive post-transition experience:
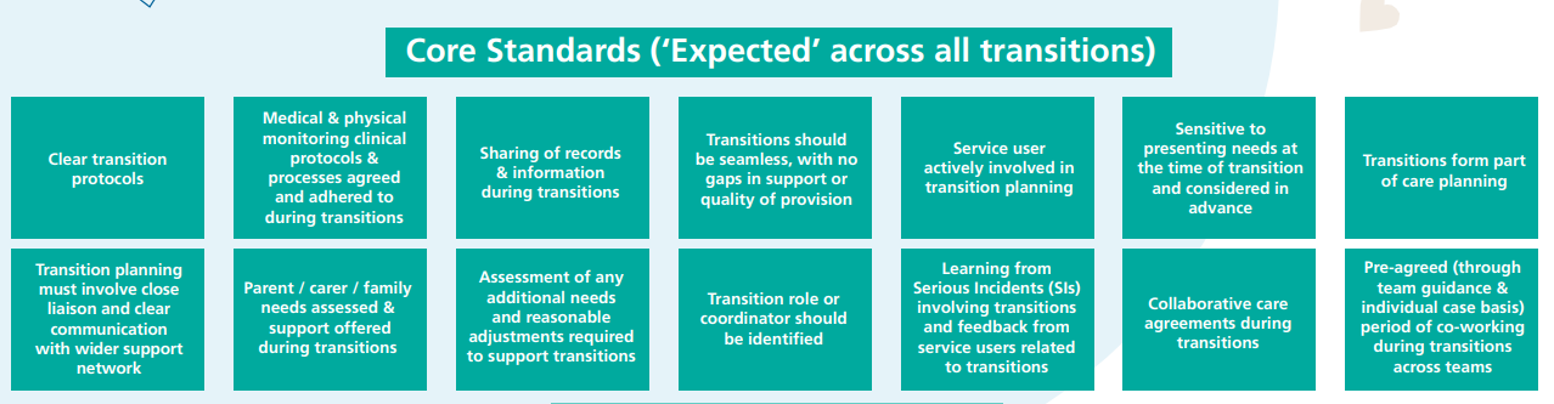
East of England NHS has developed a useful ‘Transition Standards’ guide, to help assess your service’s transition pathway and consider ways to embed these standards in practice. Click here to access a list of recommended transition standards (page 9) and a self-assessment checklist (page 41) to help with benchmarking.
There is a thriving community of eating disorders professionals on FutureNHS. Click the button below to join and access support from fellow professionals.
Visit FutureNHS