Pulmonary rehabilitation: how to assess exercise capacity and peripheral muscle strength

This learning resource provides information for healthcare professionals conducting pulmonary rehabilitation. In this module you will learn:
Why we use tests of exercise capacity and muscle strength
- How to perform field walking tests safely to measure exercise capacity
- How to perform tests of peripheral muscle strength
There is also a short quiz at the end of the module to test your knowledge.
The guidance in this learning resource is aligned with the London Pulmonary Rehabilitation Competency Framework, which was developed to support the development of a consistent approach to documenting, evidencing and developing workforce competency in pulmonary rehabilitation services. Assessing exercise capacity and peripheral muscle strength using validated outcome measures are associated with Competency 8: Objective Assessment, as set out in the framework.
What is the purpose of assessing exercise capacity?
Assessing aerobic exercise capacity using a field walking test or laboratory cardiopulmonary test is a core part of the initial assessment for pulmonary rehabilitation patients.
The test results provide a reliable indication of the exercise capacity of a patient. They can also provide insight into the ability of the patient to perform daily activities and identify any factors that may limit exercise. The results allow for the development of individualised exercise plans at an appropriate intensity for the patient. They also provide a baseline to evaluate the effectiveness of pulmonary rehabilitation following completion of the programme.
Reduced exercise capacity has been associated with health outcomes, such as increased mortality, reduced quality of life and increased risk of hospitalisation. Therefore tests of exercise capacity can also provide important information regarding disease severity and prognosis for clinicians.
How should I perform field walking tests to assess exercise capacity?
There are two main field walking tests used to measure functional exercise capacity, the 6 Minute Walk Test (6MWT) and the Incremental Shuttle Walk Test (ISWT). These are simple practical tests that can be performed easily in an outpatient setting, require minimal equipment and have been shown to be responsive to pulmonary rehabilitation. With the correct planning, either of these tests can be used to safely give a reliable indication of a patient's exercise capacity to guide exercise prescription.
The information below summarises the technical standards for the 6MWT and ISWT established by the European Respiratory Society and American Thoracic Society, which are the international agreed standard operating procedures for carrying out these tests.
Ensuring patient safety during field walking tests
Performed correctly, the 6MWT and ISWT are relatively safe tests for most patients attending pulmonary rehabilitation. However, there are some conditions which mean a patient should not take a field walking test:
Additionally, there are a number of relative contraindications for the tests. Patients with these conditions should be referred to a senior clinician for an assessment or decision regarding suitability to conduct the tests before they are undertaken:
With correct screening for the above conditions and appropriate monitoring during the tests, research suggests that very few patients who undertake either the 6MWT or ISWT will experience any long-term complications from the test itself.
However, it should be noted that maintaining oxygen saturation monitoring during the tests is extremely important and the assessor should stop the test if the patient desaturates below 80%, or reports symptoms that make continuing with the test intolerable. Both of these are acceptable endpoints for the tests and should be recorded as such.
Conducting the 6 Minute Walk Test (6MWT)
The 6 Minute Walk Test (6MWT) is a self-paced test where patients are asked to walk as far as possible in 6 minutes along a flat 30 metre track. The patient should aim to walk as far as possible in 6 minutes and should not run or jog. They are permitted to slow down, or stop and rest as necessary, but should resume walking when they are able and the timer should not be stopped during any periods the patient is paused.
Additional Considerations
Environmental factors or changes in methodology can have a significant impact on 6MWT results. In particular, the following factors should be kept consistent between tests and occasions to ensure valid comparable results:
-
-
- Course length – courses of a least 30 metres in length are recommended for the 6MWT. Studies have shown differences of in results of 50 metres or more when comparing 30 metre and 10 metre tracks.
-
-
-
-
- Course layout – cones at either end of the test track should be inset by 0.5 metres
-
-
-
-
- Use of wheeled walkers for oxygen and/or instructor-carried oxygen - if the instructor carries oxygen for the patient they should remain behind them to avoid influencing the pace of walking
-
-
-
-
- Use of supplemental oxygen – the same oxygen conditions should be used for all tests
-
-
There is evidence of a significant learning effect for the 6MWT, and therefore the test should be repeated twice (after an interval of 30 minutes) and the best distance recorded. Standardised instructions and phrases of encouragement should also be used to avoid influencing the test results.
Potential adjustments for comorbidities
For patients who need to hold anything in their hands during the test (such as a walking stick or supplemental oxygen), pulse oximeters should be positioned in such a way as to minimise interference - if possible by placing on the hand not in use.
For patients with poor peripheral circulation, you may need to use an ear probe oximeter.
Conducting the Incremental Shuttle Walk Test (ISWT)
The Incremental Shuttle Walk Test (ISWT) is a maximal and progressive walking test which gets harder as the test progresses. The patient is asked to walk progressively faster on a 10 metre track in time to a set of beeps played on a pre-recorded audio track. Access to the ISWT may be obtained from the University Hospitals of Leicester NHS Trust.
Initially, the speed is very slow, with the speed increasing every minute. The speed at which the patient should walk is directed by an audio signal. A triple bleep indicates the start of the test and whenever the walking speed is increased. The patient continues to walk until they are either too breathless, or they can no longer keep up with the beeps (defined as the patient being 0.5 metres away from the cone when the bleep sounds on a second successive 10 metre length). The total number of completed 10 metre lengths (shuttles) should be noted.
Additional Considerations
Environmental factors or changes in methodology can have a significant impact on ISWT results. In particular, the following factors should be kept consistent between tests to ensure valid comparable results:
-
-
- Course layout – cones at either end of the test track should be inset by 0.5 metres
-
-
-
-
- Use of wheeled walkers for oxygen and/or instructor-carried oxygen - if the instructor carries oxygen for the patient, they should remain behind them to avoid influencing the pace of walking
-
-
-
-
- Use of supplemental oxygen – the same oxygen conditions should be used for all tests
-
-
Similarly to the 6MWT, there is evidence of a significant learning effect for the ISWT and therefore the test should be repeated twice (after an interval of 30 minutes) and the best distance (number of completed shuttles x 10 metres) recorded. Only standardised instructions from the prerecorded audio are used. No additional encouragement is given by the instructor, with the exception of advising the patient of the need to increase their walking speed.
Potential adjustments for comorbidities
Because the test is dependent on being able to listen to both prerecorded instructions and regular beeps, it may not be possible to conduct this test for patients with significant hearing impairments. The 6MWT may be easier to perform in these circumstances.
For patients who need to hold anything in their hands during the test (such as a walking stick or supplemental oxygen), pulse oximeters should be positioned in such a way as to minimise interference - if possible by placing on the hand not in use.
For patients with poor peripheral circulation, you may need to use an ear probe oximeter.
What is the purpose of assessing peripheral muscle strength?
Assessing peripheral muscle strength in pulmonary rehabilitation helps to identify muscle weakness. Skeletal muscle dysfunction and weakness of the lower limbs, particularly the quadriceps, is a common consequence of chronic respiratory disease.
Lower limb function is important in getting up and down stairs, in and out of chairs which is important to maintain independence. Weak muscles become easily fatigued and this leads to reduced exercise tolerance, functional limitation, and disability.
For the purposes of pulmonary rehabilitation, quadriceps strength is regarded as a reliable measure of peripheral muscle strength. Testing peripheral muscle strength allows for the prescription of appropriate resistance training to target increases in muscle strength and endurance. It also provides a baseline to evaluate the effectiveness of pulmonary rehabilitation following completion of the programme.
Reduced quadriceps muscle strength has been associated with increased healthcare utilisation, exercise intolerance, reduced life expectancy and reduced quality of life.
How should I perform an assessment of peripheral muscle strength?
Although assessing peripheral muscle strength (specifically lower-limb muscle strength) is outlined as necessary in the British Thoracic Society guidelines, there is no preference for a particular type of testing in the current guidance. Therefore, a variety of different approaches to measurement are possible.
Ensuring patient safety during tests of peripheral muscle strength
Peripheral muscle strength tests, when performed carefully, help to guide accurate exercise prescription. However, these tests are contraindicated when a vigorous muscle contraction could cause further injury. Patients with these conditions should not perform tests of muscle strength:
Some patients may also have comorbidities which limit their ability to exercise. In all cases clinical judgement should be exercised. Patients with the following conditions should be referred to a senior clinician for advice before testing:
Patients with these conditions (or other illnesses affecting their ability to exercise) are also likely to need specific modifications to their exercise prescription to allow them to complete the programme.
Different ways to measure muscle strength (isometric and isotonic techniques)
There are two primary methods of testing muscle strength:
-
-
-
- Isometric exercises - static exercises where force is produced but the muscle remains the same length, and the joint angle does not change – such as a plank or wall sit
-
-
-
-
-
-
- Isotonic exercises - dynamic exercises where force is produced which changes the length of the muscle or joint angle – such as a bicep curl or squat
-
-
-
Isometric and isotonic exercise methods can both be used as valid measures of quadriceps strength. Choosing between the two may come down to two considerations:
-
-
-
- Practical availability of equipment for measurement - in some settings, tools for measuring isometric strength such as strain meters may not be available or it may not be possible to set up a reliable, repeatable test
-
-
-
-
-
- Purpose of measurement - although isometric strength has the most closely-studied relationship to prognostic information, isotonic exercises may provide more information relevant to functional tasks such as moving about the home.
-
-
The rest of this section will explain how to use different techniques for measuring quadriceps strength.
Isometric muscle strength testing
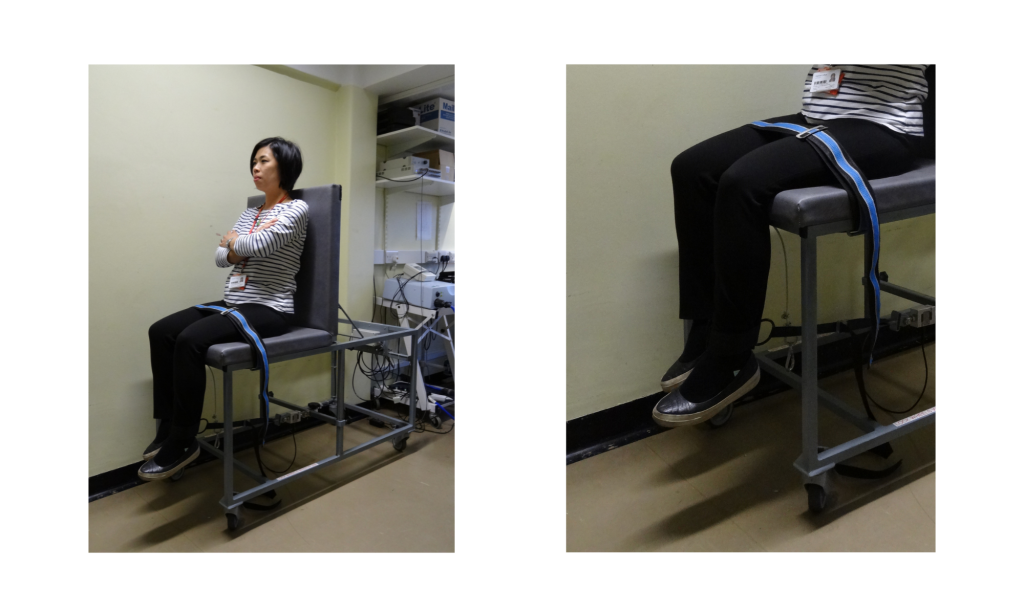
Isometric muscle strength testing uses specialist equipment such as strain meters or isometric dynamometers to test the maximum output of a muscle without shortening the muscle or changing the joint angle. The image above shows a common set-up for testing quadriceps strength using a strain meter. Use of isometric strength testing may be limited due to availability of specialist equipment and or training.
You should follow the instructions for the device you are using to set up the test. Bear in mind that differences between pieces of equipment (including how accurately the equipment is calibrated) and how the test is set up will cause significant variance in results. For example, attaching a stain meter further away from the knee joint will result in a higher level of force being recorded.
If you are using a hand-held or portable measurement device, it is crucial that it is appropriately braced to ensure it cannot move during the test.
As a general rule, you should perform a progressive warm-up and then several tests at maximal effort, recording the highest score as the result of the test. A typical test could entail:
-
- A warm-up exertion for 3 seconds at 50% of perceived maximal effort, followed by a minute of rest;
-
-
- A warm-up exertion for 3 seconds at 75% of perceived maximal effort, followed by a minute of rest;
-
-
- Three maximal effort exertions at 100% effort, with at least one minute between exertions.
-
There is no current international consensus on isometric testing approaches for pulmonary rehabilitation. You can find general guidance on isometric testing and common types of isometric testing (such as hand-held dynanometry) on Physiopedia.
Isotonic muscle strength testing
Isotonic muscle testing uses equipment such as resistance machines or leg weights to test the maximum dynamic output of a muscle. A range of commercial gym equipment (such as leg extension machines or leg presses) may be used, as well as ankle weights or other free weights.
As with other tests, it is essential that the equipment used remains consistent between tests to allow for comparisons to be made. It is particularly important to be consistent in how the equipment is set up (e.g. consistent range of motion for resistance machines where the seat, lever or other parts of the equipment may be adjusted). Make sure that the patient can complete the full range of motion for an exercise without restriction; for tests such as the seated leg extension using ankle weight shown in the video in this module, you may need to adjust the height of the chair for taller patients to ensure the floor does not limit the range of motion.
The primary output of muscle strength testing is a 1 Repetition Maximum (1RM) - the greatest weight for which a single repetition can be achieved by the patient. You may choose to either test a true 1RM or use submaximal loads to estimate a 1RM. Your choice will depend on the equipment available to you and the experience of the patient; sub-maximal testing may be safer for patients who are less familiar with resistance training.
Watch the video below to find out more about warming up for isotonic muscle strength testing and conducting these types of tests.
Use of 1 rep maximum and calculations to estimate 1 rep maximum from sub-maximal work
The strength-building elements of most exercise prescriptions use percentages of a one-rep maximum (1RM) to guide training load. For example, the prescription may call for 5 repetitions of a dumbbell shoulder press at 70% of 1RM.
1RM is used to indicate the maximum load that could be safely lifted for a single repetition. Isometric exercises can often be performed as 1RM.
However, for isotonic exercises it is generally likely to be easier and safer to conduct a sub-maximal test, where the patient lifts a lighter load for as many repetitions as they can, and then estimate their 1RM using a calculation based on the load and repetitions achieved.
The two main calculations used for this estimation are the Brzycki and Epley formulas:
Brzycki formula
Estimated 1RM = Weight lifted / (1.0278 – (0.0278 x number of repetitions))
Epley Formula
Estimated 1RM = (0.033 x number of repetitions x weight) + weight
You can also use an online calculator to perform the calculations.
Note that the two formulas give slightly different results; if you are using more than ten repetitions to estimate the 1RM, the Epley formula will return a slightly higher estimate. For this reason, it is important that the same calculation is always used when comparing scores for an individual patient.
- After reading this resource you should understand…
- Why we perform tests of exercise capacity and peripheral strength
- How to perform recommended tests of strength and exercise capacity safely and consistently
- Adjusting tests to meet the needs of your service users or physical setting
- Calculating and recording results


