E-Prescribing
E-PRESCRIBING@Imperial College Healthcare NHS Trust
Following from interviews taken with staff groups involved in the implementation of an electronic prescribing system at Imperial NHS Trust, this website contains condensed lessons and key facts which aim to aid other NHS organisations considering implementing similar solutions.
This work was undertaken by the Technology Team at the Health Innovation Network in September 2018.
Please click below to learn more about the insights that were learnt from different professions and around different themes and to download further resources. Scroll down to find out more about the implementation plan undertaken by Imperial.
PROJECT OVERVIEW
They are a Global Digital Exemplar Trust that is internationally recognised for delivering exceptional and efficient care through the use of world-class digital technology and information. Exemplars share their learning and experiences to enable other trusts to follow in their footsteps as quickly and effectively as possible.
Following the implementation of an Electronic Health Record (EHR) system in 2013, funded in part by the NHS National Programme for IT (NPfIT), Imperial decided to implement electronic Prescribing and Medicines Administration (ePMA) in 2015.
Implementation Schedule
The ePMA implementation at Imperial was rolled out alongside the Clinical Documentation software, where the implementation was undertaken in eight tranches as outlined below.
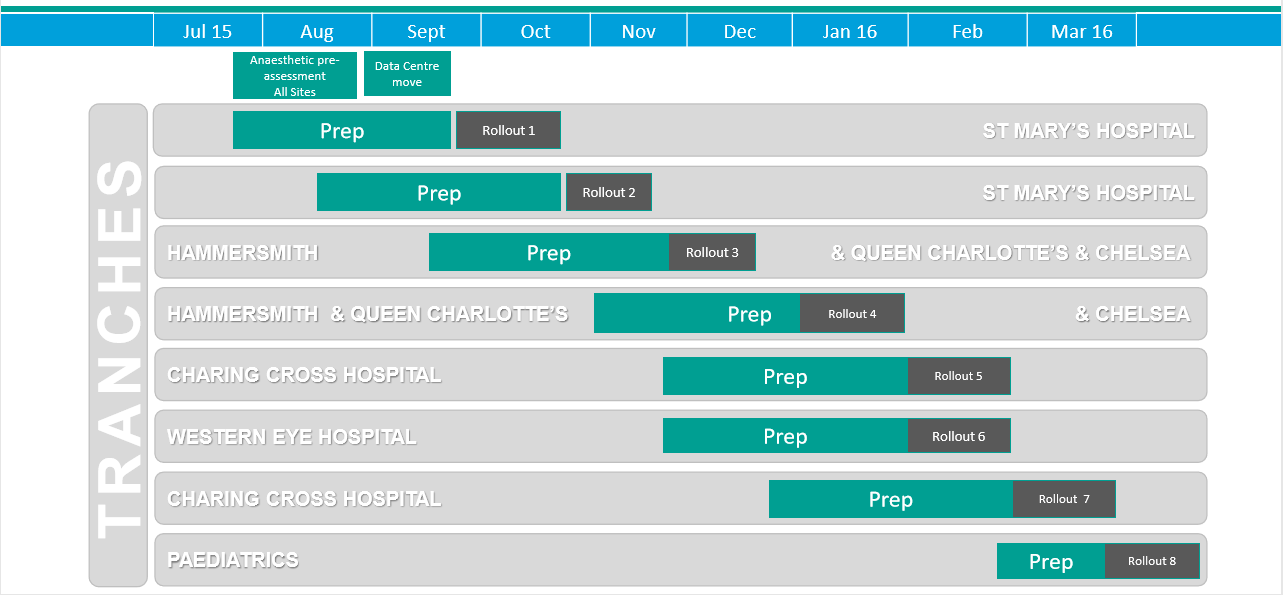
| Tranch | Preparation Start Date | Deployment Start Date | Deployment End Date |
|---|---|---|---|
| St Mary’s Hospital (1/2) | 27/07/2015 | 21/09/2015 | 18/10/2015 |
| St Mary’s Hospital (2/2) | 24/08/2015 | 19/10/2015 | 15/11/2015 |
| Hammersmith and Queen Charlotte’s & Chelsea (1/2) | 24/09/2015 | 16/11/2015 | 13/12/2015 |
| Hammersmith and Queen Charlotte’s & Chelsea (2/2) | 16/11/2015 | 11/01/2016 | 07/02/2016 |
| Charing Cross Hospital (1/2) | 14/12/2015 | 08/02/2016 | 06/03/2016 |
| Western Eye Hosptial | 14/12/2015 | 08/02/2016 | 06/03/2016 |
| Charing Cross Hospital (2/2) | 11/01/2016 | 07/03/2016 | 03/04/2016 |
| Paediatrics | 29/03/2016 | 28/03/2016 | 24/04/2016 |
“From the physician perspective, the biggest change was to the discharge prescribing”Consultant Geriatrician, Imperial College Healthcare NHS Trust
Weeks 1 - 2
Preparation Packs
Gathering information to support project delivery and identifying risks and issues. Specifically ascertaining the following:
– Bed numbers and level of care
– Staffing levels
– Existing infrastructure
– Clinical workflows
– Clinical team workflows
– Prescribing and administration workflowsWeeks 2 - 7
Infrastructure
To determine the hardware and infrastructure requirements across clinical areas (i.e. number of new computers needed), the following criteria were considered:
– Maximum number of staff in the location
– Acuity of patients
– Existing equipment
– SpaceFor further information click here.
The types of computers that were supplied were:
– Powered carts for ward rounds
– Laptop carts with drawers for drug rounds
– Laptop carts –desktop PCsWeeks 3 - 8
Smartcards
For the testing of smartcard readers, the provision of staff access and the development of a custodian system for temporary staff, the following actions were required:
– Completion of the designated training
– Identification of secure locations to store cards
– Development of local procedures for smartcard issuing and activation
– Preparation of documentation for issuing temporary accessWeeks 3 - 9+
Change management
This required working with the different clinical services to examine current processes for documenting patient records. This included both:
– Generic documentation
– Ward / department specific documentationSupporting teams to decide how to effectively use the electronic patient record was also necessary in moving forward:
– Mapping paper processes and forms to the ePMA system
– Future developmentsIdentifying benefits with services and support realisation was also part of the change management process.
Weeks 6 - 8
Training
‘Champion’ users of the ePMA system were identified and their training consisted of classroom-based sessions (half day for doctors and a full day for nurses).
The training for other users encompassed in situ familiarisation sessions, which were delivered by floorwalkers.
Other resources and tools that were available to users included videos, quick reference guides and crib sheets.
Weeks 7 - 9
Business Continuity
The Business Continuity plan was articulated around the following actions:
– Real time local copy of clinical information for patients on selected wards
– Machine identification
– Embedding of testing in day-to-day activitiesA trust-wide ePMA system downtime plan was also put in place.
End Week 8
IP Clinical Documentation Cutover
Go/No-Go Decisions for go-live to beginning on the following Monday were made on the preceding Friday.
Week 9
In-patient electronic Clinical Documentation Software Go-Live
One IT Floorwalker was deployed to each clinical area from 7.30 am.
Week 10
In-patient ePMA system Go-Live
Junior doctors would transcribe drug charts under the supervision of the Pharmacy Team.
A dedicated floorwalker supported the documentation and ePMA systems on each ward and undertook the following activities:
– Determining which patients required transcription
– Removing paper notes from the end of the bed
– Escalating issues as per defined criteria
– Scheduling checkpoint calls to track issues / monitor progressFloorwalkers were present for drug rounds and during / after ward rounds. For every four locations, one floorwalker would be on site from 11 pm to 8 am and at weekends.
Support was flexible and based on the intensity and complexity of each clinical area, which was generally determined by the:
– Number of beds
– Turnover of patients
– Acuity
– Complexity of drugs
– IT skills of staffSecond level support for ePMA was provided by the Pharmacy Team.
Week 11
Outpatient electronic Clinical Documentation Software & ePMA system Go-Live
Overnight floorwalker support was reduced as need decreased.
Week 12
Stabilisation
There were generally two tranches per hospital site, which ran sequentially. As a result, the first wave of tranches effectively received an additional two weeks of support, as floorwalkers were still on site overseeing the second wave deployments.
We're here to help
if you have any question or would like more information about e-Prescribing, please contact us.
Get in touch