Annual Review 2017/18
Improving lives
Our mission is to speed up the best in health and care. We do that to improve the lives of south Londoners. Working with our partners, we identify innovation that will improve lives and support health and care organisations to adopt and adapt it, so people can see tangible benefits from improved care. In this section of the report, we highlight some of the ways we worked to help NHS and care staff improve lives through innovation in 2017/18, across our range of clinical programmes.
Innovation and patient safety
Given the strong links between safety and organisational culture, we worked with members to promote learning cultures. We bring people with similar safety interests together to share best practice and learn from each other. For example, in March, our Patient Safety team set up a learning system that aims to make maternal and neonatal care services safer and reduce rates of maternal and neonatal deaths. NHS Improvement and fellow Patient Safety Collaborative colleagues are key partners, with the system encouraging learning across a wide range of groups.

Looking to the future, a key aspect of our maternity work will include collaborating with maternity units across south London to make the best use of evidence-based interventions, such as PReCePT (Preventing Cerebral Palsy in Pre-term Labour). As part of a national AHSN programme starting in 2018/19, this project aims to increase the use of magnesium sulphate, which has been demonstrated as an effective neuroprotectant for babies delivered prematurely. Antenatal administration reduces the risk of cerebral palsy by around 30%, however, in the UK, uptake has been significantly lower than other countries.
30%
reduction in the risk of developing cerebral palsy through taking of magnesium sulphate as an effective neuroprotectant for babies delivered prematurely.

‘The world of patient safety and experience remains full of challenge and enormous opportunity’
Read our Patient Safety Director’s reflections on the year here.
Improved way to record the agreed plan of care for a patient when their condition is deteriorating
In December, we agreed a new pilot with St George’s University Hospitals NHS Foundation Trust to develop and introduce a new Treatment Escalation Plan (TEP). This is an improved way to record the agreed plan of care for a patient when their condition is deteriorating. It is written by the most senior medical clinician looking after the patient, following a discussion with the patient and/or relative. The new system is being tested out through real-life use in the Emergency Department, Heart Failure Unit, Medical Assessment Unit and two more wards. The learning from this pilot is being used to further develop the TEP, with a plan to roll it out across the Trust and find opportunities to spread its uptake elsewhere. The work was led by one of our Darzi Fellows.
Supporting staff through Communities of Practice
In line with the clear links between culture and safety, the Patient Safety team led a variety of workshops and Communities of Practice in 2017/18. In total, three staff-wellbeing orientated Communities of Practice ran throughout the year: Staff Wellbeing, Speaking Up, and Duty of Candour. These Communities supported the wellbeing of staff, but also their experience of the workplace, how comfortable they feel admitting mistakes and speaking up when they feel that it is necessary.
‘Conversation of equals’ puts patients views at the centre’
Read more from Jane Hopkin, a patient member of the HIN Community of Practice here.

local pharmacists in Lewisham taking part in our new Transfer of Care Around Medicines
Working with Community Pharmacists to minimise the risk of errors
In March, we adapted an innovative approach to refer patients from hospital to their Community Pharmacist for support with new, existing and changed medicine regimes. Community pharmacists are well placed to reduce the safety risks that can arise when people move between care providers or return home from hospital. More than 50 local pharmacists in Lewisham signed up for the new “Tranfer of Care Around Medicines”, starting with referrals from University Hospital Lewisham, part of Lewisham & Greenwich NHS Trust. They liaised with hospital pharmacists and GPs to provide a range of advice and support services to help people manage their medicines confidently and will continue to do so throughout 2018/19.
Raising awareness of sepsis
Sepsis is responsible for 44,000 deaths in England each year and research shows that a third of these could be avoided if care-givers or health professionals recognised the signs and treated the condition faster. To help address this, the Patient Safety team released Spotting the Signs of Sepsis, a series of awareness films, in partnership with ASK SNIFF, the Sepsis Trust NHS England and NHS Choices. The films were co-designed with ASK SNIFF’s Parent Panel and the project shortlisted for the 2018 HSJ Patient Safety Awards. The lead film has been viewed more than 2.8 million times, with one mother getting in touch to tell us that she felt that the video had given her the information she needed to recognise sepsis, and save her daughter’s life.

‘If it wasn’t for your video, I wouldn’t of taken my daughter to A&E at 2 in the morning’
Read more from one mother who viewed the film and took quick action here.


Preventing strokes in south London
Stroke can have a devastating effect on people’s lives and carries a high financial cost to the NHS. Yet official figures show that more than 420,000 people across England have undiagnosed irregular heart rhythms, including an estimated 60,000 Londoners, which can cause a stroke if not detected and treated appropriately. For this reason, our Stroke Prevention team worked with other AHSNs around the country to ensure the NHS has access to the latest digital devices to detect irregular heartbeats. The team kicked off the project during a national awareness week, offering Londoners free pulse rhythm checks in various healthcare settings, including hospitals, GP practices and local pharmacies, and were supported by the Mayor of London and others. In February, the team distributed a range of digital devices to NHS staff in south London so that they could conduct fast and accurate pulse rhythm checks on Londoners on an ongoing basis, including a smartphone-linked device that works via an app and a new blood pressure cuff that also detects heart rhythms. Small and easy-to-use, NHS staff can also take the devices on home visits. The programme is part of a national AHSN project to distribute 6,000 devices – funded by NHS England – and is expected to prevent 3,650 strokes, save 900 lives and save £81 million annually.
Using new tech to prevent strokes in South London
Read Alex’s story about the potential of technology to detect Atrial Fibrillation here.

Dementia tool helps spot sings of disease
Dementia is one of the main causes of disability in later life with around 850,000 people estimated to be living with the condition, many of whom are aged 65 years or over. Early diagnosis of dementia can save up to £6,254 per person, according to Age UK. In 2017, the Healthy Ageing team adapted its ‘DeAR-GP’ memory observation and assessment tool for use in housing and community health settings. DeAR -GP is currently being piloted with the support of the Alzheimer’s Society in HMP Parkhurst Prison and there are plans to pilot also in community pharmacy settings. This simple effective tool has multiple possibilities across different settings, ensuring people who may have dementia are identified, enabling them to maximise choice and control over their lives.
Integrating mental and physical health
We work hard to ensure that mental health is embedded across all of our projects. For example, ensuring that our diabetes programmes address mental health as well as physical health and through the inclusion of AF testing in secondary mental health settings.
In 2017 we also developed a new mental health lead role. This role will focus even further on acknowledging the psychological impact of long term conditions and the need to ensure people with severe mental illness also benefit from our innovation programmes.
One of the first projects identified to spread across London in 2018/19 is the Serenity Integrated Mentoring (SIM) Programme developed by Paul Jennings NHSE Innovation fellow. The programme involves specially trained Metropolitan Police officers holding an NHS honour contract so that they can work alongside NHS mental health care coordinators to mentor individuals, supporting them to find new ways of coping and managing with their mental health. Mentoring has been proven to address the practical, social and emotional issues that contribute to a mental health crisis, resulting in fewer detentions under Section 136 and more proactive support for individuals.

‘Holistic approach to ageing sees new focus on vision to prevent falls and new tech to share urgent medical records’
Read more from Rebecca Jarvis, Healthy Ageing programme director on how we’re supporting the health of older people in south London here.
Improving the lives of south Londoners with diabetes
Diabetes care and prevention of Type 2 diabetes continued to be a priority area for the NHS in 2017/18. Across our partners in trusts and CCGs, approximately £3 million of investment was secured from NHS England for south London. Working with partners, we supported a wide range of projects, including:
• The creation of a brand new diabetes education booking service which will support people with diabetes to access the right self-management support at the right time for them, with fully integrated psychological support. This service will go live for patients in Autumn 2018.
• The “Think Diabetes” programme which turns the spotlight onto the responsibilities of employers in south London to provide top quality support to their employees who have diabetes.
• A new online training package for healthcare professionals in primary care, with 4,000 user licences available for south London staff.
• The Youth Empowerment Skills (YES) programme for 14-19 year olds (pioneered at Guy’s and St Thomas’ NHS Foundation Trust) will be available for young people from all over south London with Type 1 diabetes from summer 2018.
• New multidisciplinary foot clinics for people across south east London and Kent – these vital services will accelerate patients’ access to specialist multidisciplinary foot care, prevent amputations and improve quality of life as well as delivering considerable savings to the local NHS.
Type 2 diabetes prevention also progressed throughout the year. Commissioned by Southwark CCG, we led the local health economy partnership for Healthier You – the national diabetes prevention programme (DPP). Healthier You is a nine month group-based programme which supports people to make the lifestyle changes needed to reduce their risk of developing Type 2 Diabetes.
Over
12,000
South Londoners have now been referred to Healthier You by GPs and NHS Health Check Providers and south London has one of the highest conversion rates to attendance at the initial session in the country (60%).
By the end of 2017,
584
more people with Type 1 diabetes were using pump therapy as a result of our Diabetes Improvement Collaborative and the ongoing commitment of south London diabetes clinicians.
Innovation in chronic pain management
The Musculoskeletal (MSK) team continued to pioneer an alternative and highly effective solution to joint pain management, ESCAPE-pain (Enabling Self-management and Coping with Arthritic Pain). A six-week rehabilitation programme for people with chronic joint pain, it integrates educational self-management and coping strategies with an exercise regime individualised for each participant. ESCAPE-pain grew significantly throughout the year, from 31 to 60 sites. The programme is an effective alternative to highly addictive, and often ineffective, painkillers and is proven to reduce pain, improve mental health as well as reduce healthcare costs.
To support the rapid spread of the programme the ESCAPE-pain team also created a highly successful and popular training programme that supports clinical staff and fitness professionals delivering the programme, whether they are in traditional therapy settings or in the community. Throughout the year, around 150 professionals attended the training programme, with high levels of satisfaction reported and further sessions planned for the coming year. During the year, it was decided that ESCAPE-pain would become an AHSN national programme, meaning it will receive dedicated AHSN support across the country.

2,500
participants in 17/18, which represents savings of over £4 million
‘My life has changed massively’’
Read about how ESCAPE-pain changed Arlene Rowe’s life here.


‘ESCAPE-pain offers people the opportunity to take control of their condition’
Read about Andrea Carter, Programme Director of the Musculoskeletal Clinical team’s reflections on the first five years of ESCAPE-pain here.
The MSK team also developed and tested a new model of care, called Joint Pain Advisors, for knee and hip pain. It is an early intervention for people with joint pain that provides rapid access to advice through a series of face-to-face consultations between the joint pain Advisors and people with hip and/or knee osteoarthritis. Patients discuss their lifestyle, challenges and goals and reduced the need for GP visits. They jointly develop a care plan which includes tailored advice and support based on NICE guidance. Joint Pain Advisors spread to Lewisham and Greenwich in 2017/18, with plans for Merton, Croydon, Bromley and Shropshire Public Health to launch shortly.
‘The more I exercised, the less it hurt’
Read about Chris Smith’s experience of the Joint Pain Advisor service in Greenwich here.

Working with care homes to improve transfers of care and train tomorrow’s leaders
Our team works across the NHS and care system. Examples of our work to support care homes and their staff in 2017/18 include:
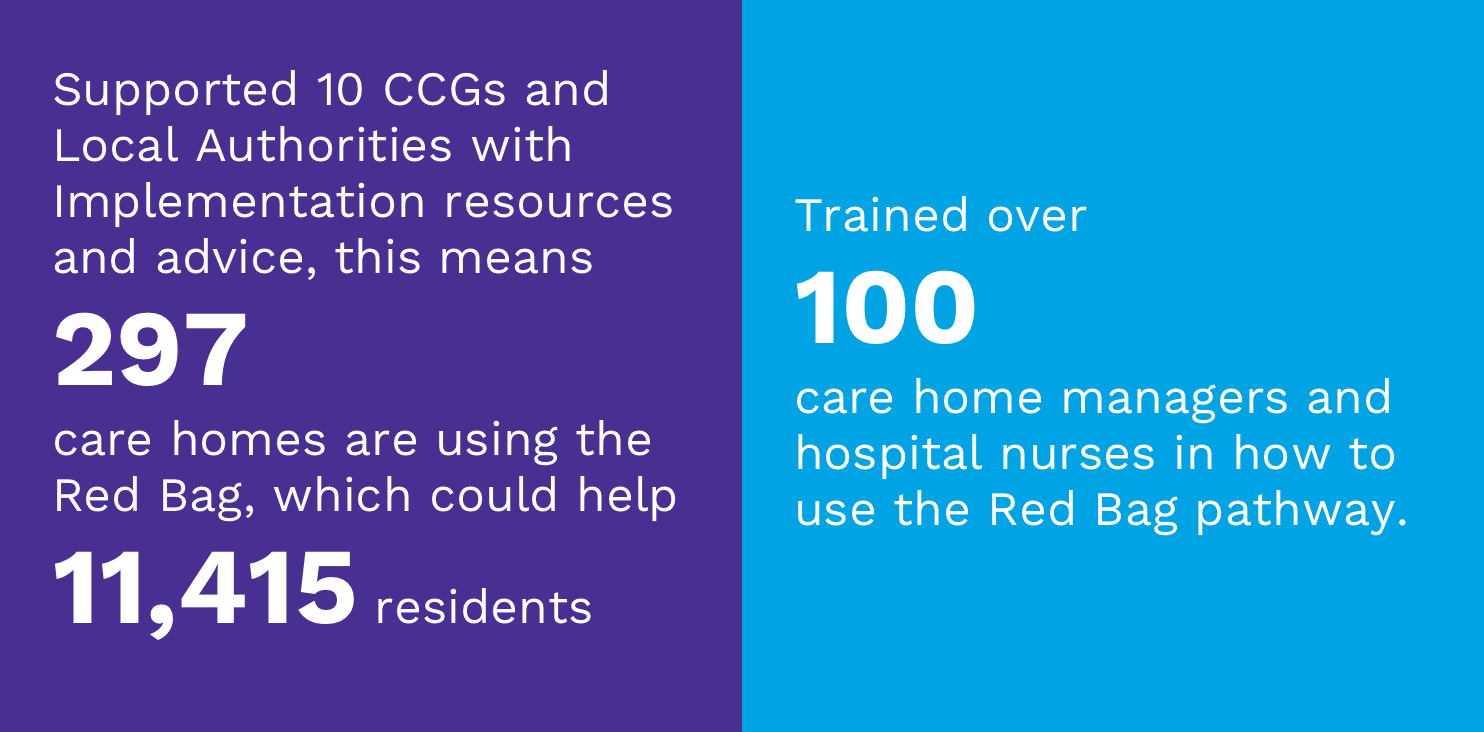
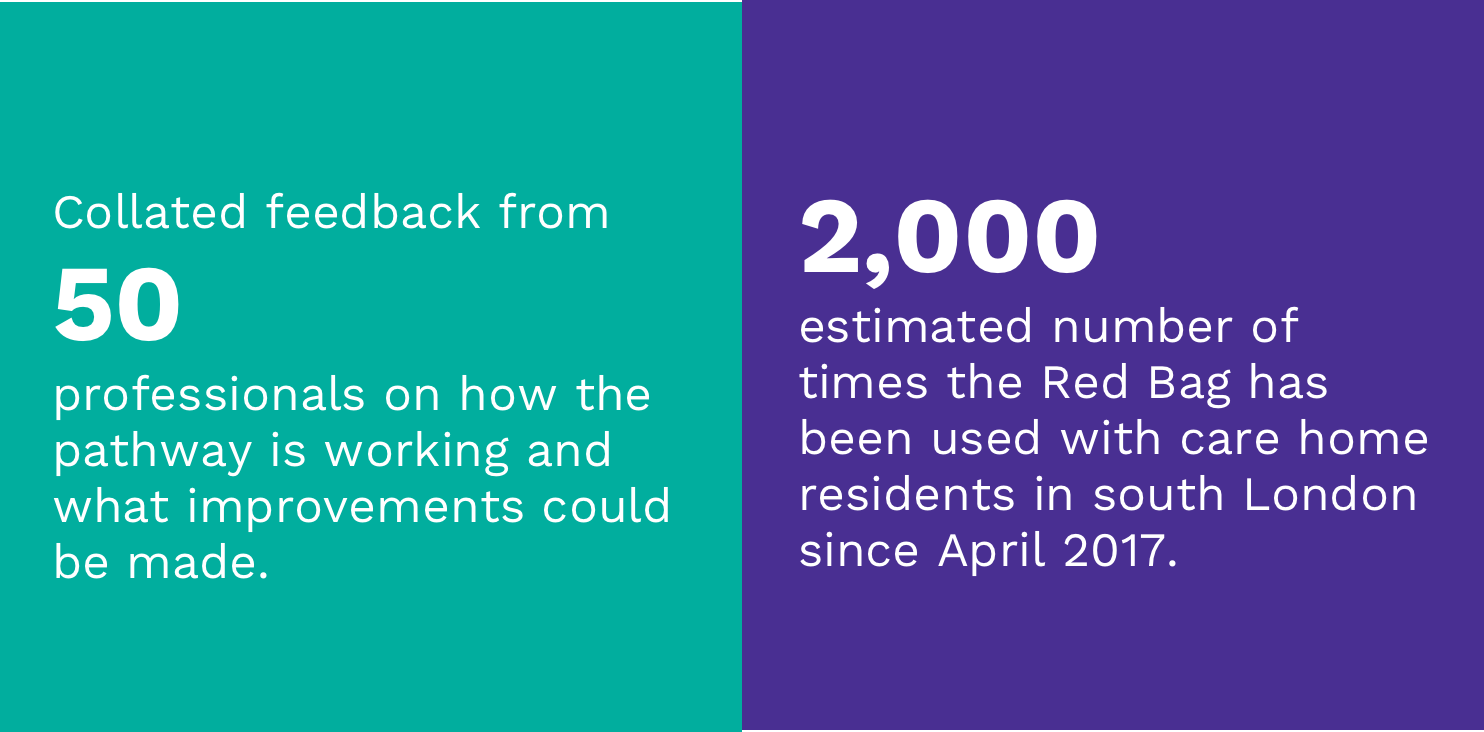
Our Healthy Ageing team supported the spread and adoption of the Red Bag pathway in 10 boroughs in south London during the year. The Red Bag is a simple innovation which ensures records and personal belongings are kept safe when a care home resident is transferred into hospital. First developed by Sutton CCG Homes of Care Vanguard, a resident’s Red Bag goes with them to hospital in an emergency and contains:
• General health information, including on any existing medical conditions
• Medication information so ambulance and hospital staff know immediately what medication they are taking
• Personal belongings (such as clothes for day of discharge, glasses, hearing aid, dentures or other items)
The Red Bag also clearly identifies a patient as being a care home resident and provides hospital staff with the information they need to speed up clinical decisions. This means patients can often be discharged sooner which is better both for the residents and for the NHS, as it means individuals are out of hospital more quickly and money is saved. Previous evaluations have found the scheme reduces length of stay in hospital by an average of 2.4 days per admission.
Our work included advice, training and facilitating for CCGs, local authorities, provider leads, the London Ambulance Service and care homes on how to implement the different elements of the pathway and how to use the standardised paperwork and monitoring tools developed by Sutton Vanguard. Toward the end of the year, we also took on responsibility for evaluating the impact of the pathway in three south London boroughs, Richmond, Kingston and Lambeth.
15
number of care home managers from 11 south London boroughs taking part in the current Pioneer Programme.
Drive to help care home managers tackle complex issues
The Healthy Ageing team and My Home Life joined forces to design and offer south London Care Homes managers a new, free leadership support and professional development programme to advance their skills, facilitate personal growth and enable them to effectively manage the complex everyday issues that impact on the quality of their service. Called the Pioneer Programme, fifteen enthusiastic and committed care home managers were recruited in the year and began the course in January 2018.