Annual Report 2018/19
When we consider innovation and transformational change in healthcare, the problems and issues we encounter are often complex, ambiguous and ill-defined, with no clear solution. Potential outcomes are new and so unknown. Solutions in one part of the system may well lead to unintended consequences in another. To approach these challenges, we need to think differently about problem solving. We must use the diversity within healthcare to problem solve and we can only do this by breaking down our silos, talking to people and seeing situations through the eyes of others.
Since 2015 at the Health Innovation Network (HIN), we have been successfully developing communities of practice (CoPs) to help meet this enormous challenge and in 2018-19 this work grew massively.
What Are Communities of Practice?
Communities of Practice (CoPs) are self-organising and self-governing groups of people who share a passion for their field and strive, through collaboration, to become better practitioners.

In the NHS, “a CoP differs from a delivery network because members are self-invited, and the ways of working are informal…it’s a conversational relationship of peers who want to share and learn from each other. They also help… develop cross boundary relationships with leaders in other parts of the organisation or community.”
From the Improvement Leaders’ Guide, by the NHS Institute for Improvement and Innovation
We currently support a number of CoPs and are always encouraging new communities to form. They include:
• Medicines Optimisation
• Diabetes in Pregnancy
• Catheter Care
• Speaking Up
• Cancer Care (four different communities)
• Learning from Deaths.
With wide representation often covering the whole health system, each community is owned by its own members who decide on the focus and the content of the learning that takes place in the community. This cuts through hierarchy and bureaucracy and helps people to learn from and with each other about what works, what doesn’t and why.
Year-long experiential learning programme launched January 2019
At the HIN we are keen to nurture new CoPs, empowering them to self-form, self-define and develop, and we are committed to supporting current and future conveners.

In January 2019, we began our partnership with the Health Foundation’s Q Network, to design and deliver a year-long experiential learning programme to provide all the building blocks for successful CoP leadership. This national Communities of Practice Leadership Development Programme is intended to help many more communities thrive across multiple issues and institutions, creating a Community of Communities that can aid them to discover one another and link their practices to ensure synergies are created wherever possible.
Between January and March 2019, we delivered the first two modules of this programme.
London Community of Practice focussing on Diabetes in Pregnancy convened in June 2018
Diabetes in pregnancy requires close monitoring to avoid adverse outcomes for mother and baby. To respond to the growing pressure on the system and to improve the health and care for these women and babies the Health Innovation Network (HIN) helped convene the Diabetes in Pregnancy Pan-London Community of Practice (CoP) in June 2018.
“It was great to have Myron Rogers with us – such an inspiration and a real trail blazer. Understanding what others were trying to do in this space, across many different roles, was also really interesting and helpful.”
“The focus on a shared interest is really powerful, and not what I had considered”
“Thank you for all for this engaging and inspiring programme”
“It has given me more tools that I can use within my own communities of practice and given me more confidence that I do not need to have all the answers but that we are all in it together”
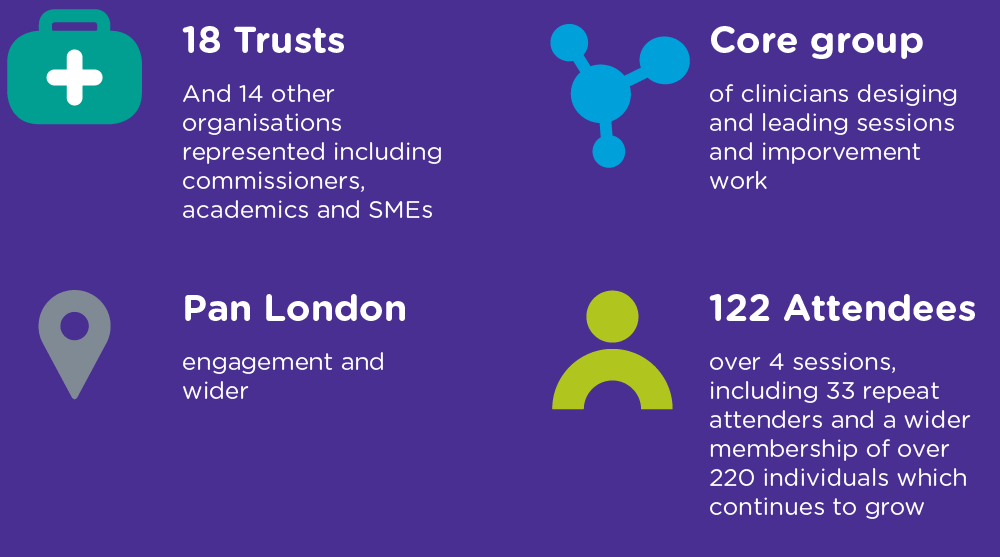
We know that in the UK many women with diabetes in pregnancy (pre-existing or gestational diabetes) experience suboptimal care and poorer outcomes. Therefore, the need for improvements in care in this area is great. Identification and management of diabetes in pregnancy is currently recognised as a priority nationwide. In London, we know that clinical services are facing real challenges in the context of growing pressures and financial/capacity strains, so finding better ways of working is vital to improving health care and outcomes of these women and babies.
Bringing together colleagues from across organisational and professional groups, the CoP aims to take on these challenges and improve care and services for women and babies across London.
The HIN can act as a neutral facilitator in the health care system (being neither provider nor commissioner) and has expertise in networking and creating collaborative change, as well as experience of working in both diabetes and maternity. We are therefore, well placed to develop and support improvements in health in this area.
In the last year, the CoP has established a number of programmes of work including:
- creating a dedicated space for diabetes specialist midwives to connect and share practices
- Supporting the adoption of technology to improve the management of diabetes in pregnancy
- leading the way in understanding practices and outcomes for women presenting with gestational diabetes post 34 weeks gestation (to support reduced variation and improved care across London)

“We have the enthusiasm and we need to keep going – participant June 2018 The only way to do it is together”
Participant February 2019
More information:
The British Journal of Diabetes, Findings of a nationwide survey of the diabetes education and training needs of midwives in the UK: