Annual Report 22/23
Speeding up the best in health and care, together
Welcome to the HIN Annual Report for 2022/23!
Watch our welcome video to hear from recently-appointed Lived Experience Partner Faith Smith, Chair Hitesh Thakrar and Chief Executive Rishi Das-Gupta.
Read on to find out more about the projects we've worked on over the last year.
1Accessing innovations
AHSN Early Intervention Eating Disorder National Programme
The HIN led the National Early Intervention Eating Disorders (EIED) programme from April 2020 to March 2023. The model used is First Episode Rapid Early Intervention for Eating Disorders (FREED), an innovative service enabling people aged 16 to 25 who have had an eating disorder for three years or less to get rapid and specialised treatment. FREED, developed by South London and Maudsley NHS Foundation Trust and Kings College London (SLaM/KCL) with initial support from the Health Foundation and National Innovation Acceleratory (NIA), was chosen as an AHSN programme for national spread and adoption in 2020.
The National EIED programme, in partnership with SLaM /KCL, has successfully led to the adoption of and implementation discussions for FREED within the footprint of every eligible Mental Health Trust in England. FREED services recruited 55 FREED Champions into specialised early intervention roles and have treated over 2,000 patients since the programme began in 2020. Going forward FREED is set to continue, led by the team at SLaM/KCL with support from NHSE.
A video to support recruitment into FREED Champion roles has also been produced, which can be viewed below.
Recruited
FREED Champions
Treated over
patients
Accelerating access to products benefitting over 500 patients in 22/23
This year saw the successful conclusion of the NHS Accelerated Access Collaborative's (AAC) Rapid Uptake Products (RUP) programme, and the launch of new activity focussed on addressing healthcare inequalities. The Innovation for Healthcare Inequalities programme, co-developed with the local system in the autumn, magnifies the spread of select technologies from previous programmes and has particular focus on the populations in the Core20PLUS5 strategy.
In the second and final implementation year of the RUP respiratory programme, a further 195 patients gained access to a novel monoclonal antibody therapy for severe asthma. People with severe asthma experience attacks despite usual treatments of inhaled steroids. While there is a group of medicines prescribed in severe asthma centres designed to address these attacks, 72 per cent of potential severe asthma patients had no referral or specialist review in the year before the RUP programme. The Asthma Biologics toolkit has been developed to help clinicians to identify severe asthma patients and direct them to the help they need. The growth in access to this therapy is expected to prevent over 200 additional severe exacerbations each year, subsequently creating annual savings of over £700k for the health system.
As part of RUP, 23 new FeNO diagnostic devices, which were introduced this year, have already supported the diagnosis of asthma in roughly 500 patients. FeNO helps to enable faster and more accurate diagnosis of asthma by measuring fractional exhaled nitric oxide in the breath of patients, which is an indicator of the level of inflammation in the lungs.
Implementation continued for the first round of products on the MedTech Funding Mandate Programme. All eligible hospitals are now either using, or in the process of adopting, a clip to secure percutaneous catheters, a test for preterm pre-eclampsia and a non-pharmacological solution for cluster headaches. In the video included in this section of our report, clinicians from the neurology teams at St Thomas’ and King’s speak about the benefits of the programme and the one of the products, ‘gammaCore’, a non-invasive treatment for cluster headaches.
Implementation of the second round of MedTech Funding Mandate products will continue through 23-24.
Maternity and Neonatal Network
The HIN has found great benefits from working with Darzi fellows over the years in partnership with our local member organisations. The Darzi fellowship supports clinicians who are looking to explore a challenge in depth to develop long term, sustainable solutions.
Between September 2021 and October 2022, Darzi fellow and midwife by background, Rosie Murphy, undertook work in Croydon to explore the inequalities that women and birthing people from Black, Asian, or mixed ethnic backgrounds experience during their maternity journey.
A series of interviews with people who experience these inequalities identified the most common themes as access barriers and failure to listen to women and birthing people. Working in partnership with the HEARD (Health Equity And Racial Disparity) campaign, Croydon NHS Trust, South West London Local Maternity and Neonatal System (SWL LMNS), the HIN and other passionate people looking into perinatal equity, Rosie hosted a “Whose Shoes” event to engage interested citizens and wider health and voluntary sector staff, to establish a network and start discussing solutions.
Rosie has written a series of blogs discussing her journey, key findings and recommendations. To further this research, the HIN, in partnership with SWL LMNS, recruited another Darzi fellow for September 2022 to October 2023. Ella Caine, also a midwife and university lecturer by background, has been working on improving interpreting services for Black, Asian and minoritised women and birthing people. Ella is planning on setting up a series of listening events across SWL with key stakeholders to understand barriers and facilitators to using interpreters and experiences of the process.
The picture board below recaps the informal discussions that were had during the “Whose Shoes” event, highlighting the topics that members felt were important to address.

Maternity and Neonatal Quality Improvement (QI) collaborative
The South London Maternity and Neonatal QI collaborative was set up in June 2022 to bring together frontline clinical and managerial staff in maternity and neonatal care to deliver a learning programme to build practical QI skills, confidence and cross-unit connections. The focus of the series is to improve the opportunities to optimise and stabilise the outcomes of the preterm infant through the seven interventions recommended by the British Association of Perinatal Medicine (BAPM).
Multidisciplinary teams from across south London, ranging from patient safety midwives and neonatal physicians to preterm birth champions, obstetric consultants and theatre staff at a range of different levels have come together to learn how they can improve the care they deliver to women and babies locally. Visiting teams on site and helping them to map out their activities and processes has been beneficial to understand the gaps and areas for improvement. The accompanying photo is from a successful process mapping session with our maternity and neonatal colleagues at St George’s NHS Trust.
The series has shown the importance of cross-unit working, learning and collaboration between teams and hospitals. Practical recommendations of best practice are now being clearly communicated across teams through posters, message of the week, simulated practice and training which has resulted in significant improvements in outcomes for preterm babies. Find out more about the series, slides and recordings. A newly developed dashboard by the National Maternity and Neonatal Patient Safety team demonstrates the local impact of the optimisation QI series and dedicated work from our staff across south London.
645 women giving birth at less than 30 weeks of gestation received magnesium sulphate within the 24 hours prior to birth. This means that 17 babies will not develop cerebral palsy.
20 women in preterm labour at less than 34 weeks of gestation receive intravenous intrapartum antibiotic prophylaxis to prevent early onset neonatal Group B Streptococcal (GBS) infection irrespective of whether they have ruptured amniotic membranes. This means that two babies were born without group B strep.
Between 14 and 23 babies born at less than 34 weeks gestational age survived because their umbilical cord was clamped at or after one minute after birth.
*
Data from April 2020 to Oct 2022
Improving chronic pain management by reducing harm from opioids
(Medication Safety Improvement Programme)
The HIN is one of fifteen patient safety collaboratives in England that has worked across the system to improve chronic pain management by reducing harm from opioids. This was done as part of delivering a National Safety Improvement ambition which aims for medication safety to have:
fewer people prescribed oral or transdermal opioids (of any dose) for more than three months.
Of the 30,000 above, 4,500 of these people will have been prescribed a high dose (>120mg day oral morphine equivalent).
In October 2022, our CPD-accredited Opioid Stewardship Quality Improvement Collaborative was launched to develop the skills and knowledge of GPs and pharmacists in safe opioid use and quality improvement processes, while at the same time receiving support to design and test change ideas to improve chronic non-cancer pain management in their own practice.
Thirty-five clinicians working in general practice and primary care networks have since enrolled onto the programme. To ensure involvement is part of our medication safety improvement workstream, we are working in partnership with over thirty people living with chronic pain and health and care professionals, combining to leverage the success of local improvements to ensure services are responsive to patients’ wishes in south London. You can find out more about our work to improve chronic pain management here:
Access Denied report
The Access Denied Report published in October 2022 was developed to address how we could transform care pathways equitably in an increasingly digital world. The roundtable discussion explored health inequalities in the context of developing and implementing digital health innovations so that we could further the discussion and understanding of this critical and complex issue.
It was attended by 17 participants who represented expert views from across industry, academia, the voluntary and charity sector, healthcare providers and commissioners.
In the report the HIN made the following recommendations for designers and developers of digital tools, and the NHS organisations who select and implement them:
- Work with digital innovations that meet the highest standards for accessibility and usability.
- Test digital products and services thoroughly with a cross section of patients, providers and commissioners.
- Use data to optimise and improve delivery to improve outcomes and minimise exclusion over time.
- Understand how different people may need specific channels of delivery at different times or for different services.
- Ensure you capture data so you can measure and compare outcomes and experience by channel.
- Don’t plan care pathways for the majority – ensure it is optimised for those from minority backgrounds too.
- Consider the support needed to move people to digital pathways.
- Ensure equality impact assessments for transforming care pathways pay attention to digital exclusion as a potential risk of inequality.
These findings were subsequently shared at the Health Excellence Through Technology (HETT) Conference contributing to the wider discussion of the evolution of patient safety in the digital era.
We would like to thank all those who attended the roundtable and shared their valuable insight.

National Blood Pressure Optimisation and National Lipid programmes
We delivered a series of national programmes around cardiovascular disease and significantly built on these to address specific local needs.
The National Blood Pressure Optimisation and National Lipid programmes were delivered with local partners to support detection and optimisation for hypertension, lipids, and familial hypercholesterolemia.
Within south west London the HIN delivered the South West London Hypertension and Lipids Forum, working closely with the ICS and the SWL Training Hub. Key statistics:
- eight sessions delivered
- 689 attendees across the sessions–average attendance of 86 people
- 38 Primary Care Networks (PCNs) supported
Within south east London the HIN worked with Clinical Effectiveness South East London (CESEL), and the South London Cardiovascular Network to support PCNs in their delivery of hypertension care. Thirty-four of thirty-five PCNs in south east London have signed up to participate in order to improve the detection and management of hypertension care, reduce inequalities and support Covid-19 recovery. The partnership with CESEL and the South London Cardiovascular Network obtained ICS inequalities funding for participating PCNs, and commissioned Mabadiliko Community Interest Company (CIC) to codesign culturally sensitive, community-based hypertension testing protocols with residents and health care professionals.
In lipids we have worked with17 PCNs across south London to test new approaches to lipid management and familial hypercholesterolaemia in primary care. We have supported over 70 per cent of south London PCNs to work on lipid optimisations. The HIN also supported successful bids for lipid transformation across our patch for a total of £586K.
We have supported over 70% of PCNs across south London to work on lipid optimisations.

2Improving outcomes
You and Type 2
Since 2018 the HIN has worked with NHS South West London Clinical Commissioning Group to develop “You & Type 2”, a personalised care and support planning pathway for people living with type 2 diabetes.
This work involved two strands – risk stratification and You and Type 2 @Home - which had to be adapted during the Covid-19 pandemic. We evaluated both in 2022.
Risk Stratification
We developed a risk stratification framework which consolidated general and disease-specific criteria to focus on people who are at high risk of developing the complications of type 2 diabetes, but not currently under secondary care management. Using search criteria that could be run through EMIS, a list was created for GP practices of people at high risk for follow-up. This was designed to allow practices to target their resources appropriately.
While the search criteria successfully identified high risk people within practices, it also highlighted significant barriers to pathway implementation at a practice level. These were predominantly linked to pressures on primary care due to the Covid-19 pandemic, and the continued challenges faced by our workforce.
You & Type 2 @ Home
The pandemic caused many routine health checks to be paused, including annual diabetes care reviews. However, with the help of remote technology providers Thriva and Healthy.io, a remote testing pathway was developed. People with diabetes received a free home blood testing kit, urine kit and blood pressure machine in the post. A care planning phone call then allowed for seven of the eight key care processes to be completed remotely.
Staff found the remote pathway useful and saw potential to reduce pressures on primary care. Many of the service users found the tests acceptable for use, with some wanting to use the pathway annually.
CVD Fellowship
In April 2022 the HIN introduced a Cardiovascular Disease (CVD) Prevention Fellowship Programme for primary care clinicians in south London with the aims to:
- enhance the clinicians’ knowledge of CVD prevention with CPD-accredited learning
- develop skills to improve the delivery of care in their practice or Primary Care Network (PCN).
The fellowship included clinical education led by local clinical experts, Quality Improvement (QI) training, and a requirement for the Fellows to deliver a QI project in their surgery/PCN, to put their new skills and knowledge of CVD prevention into practice.
The first cohort delivered significant benefits for primary care clinicians and patients in south London, as showed in the project case-studies pack, the participants’ video and animated infographic.
CVD Prevention fellowship key achievements:
primary care clinicians completed the programme

education sessions delivered

quality improvement projects delivered, covering a PCN population of
agree they feel more confident in delivering care to patients at risk of CVD as a result of the CVD Prevention Fellowship
The Fellowship Programme was part of a wider CVD Prevention programme of work. We worked with PCNs across the region to improve the management of cholesterol, high blood pressure and broad CVD risks, plus increase detection of Familial Hypercholesterolaemia and adoption of novel therapies. We continue to deliver CVD Prevention training for primary care via the SWL Lipid and Hypertension Forum.
MSK Improvement Network
In 22/23 we hosted two MSK Improvement Network events, building on the success of our previous MSK Improvement Forum and Back Pain Forum.
The events - held at St Thomas’ Hospital – were attended by clinicians and leaders working in musculoskeletal services across London, and proved fertile ground for colleagues to discuss improvement and innovation.
Chaired by Ben Wanless (Consultant Physiotherapist, St George’s University Hospitals NHS Foundation Trust) and Christina Sothinathan (NHS Navigator and Fellow, DigitalHealth.London and Advanced Practice Physiotherapist), delegates were able to hear from a range of speakers and perspectives including Dr Ian Bernstein, GP and Regional Clinical Director for Musculoskeletal services, NHSE (London).
Presentations included topics such as shared decision making, the role of supervision and leadership in healthcare and updates on Regional MSK improvement projects. With musculoskeletal conditions accounting for the largest proportion of people on NHS waiting lists, it was great to see such good turnout at the events, enthusiastic debate in interactive sessions, and new connections being made.

Whole Schools Approach to mental wellbeing
in south west London
South West London Integrated Care System has worked with schools and colleges since 2018 to provide earlier support for children and young people’s mental health. In its independent evaluation, the HIN Insights team gathered feedback from 422 stakeholders, including teachers, mental health service providers, children and young people, parents and carers. These stakeholders provided considerable qualitative evidence of positive change associated with the programme in all eight Whole School Approach domains.

Figure 1 Eight principles to promoting a whole school or college approach to mental health and wellbeing[1]
[1] Source: Public Health England working with the Department for Education (2021) Promoting children and young people’s mental health and wellbeing. A whole school or college approach. HM Government. Link
Evidence from quantitative data demonstrates a good deal of new activity aimed at improving emotional wellbeing in schools. Though limited in quantity, clinical outcomes data indicates improvements in pupil and staff wellbeing following introduction of the Programme.
SWL ICS welcomed the evaluation report and has already acted on some of the recommendations, such as addressing the issues identified with quantitative success measures. There is an action plan in place to take forward our recommendations.
In the first quarter of 2020/2021,
children and young people accessed mental health support through the Kooth online platform

Figure 2: Quarterly average number of referrals to each Mental Health Support Team (n = number of quarters data was available for). Source: SWL Integrated Care Board and the Mental Health Support Team Providers: SWL and St Georges NHS Foundation Trust (SWLSTG), Achieving for Children (AfC), South London and Maudsley NHS Foundation Trust (SLaM) and Off the Record (OTR).
Mental Health Safety Improvement Programme
The programme aims to improve safety and experience in mental health wards by reducing restrictive practices such as physical restraint, seclusion, and rapid tranquilisation by 25 per cent. Across the south London mental health trusts, the HIN has worked with seven patient wards by enabling shared learning, systematic quality improvement, codesign and coproduction and awareness of health inequalities.
Through a proactive steering group and local experts by experience, the programme designed an interactive platform (Patient Safety Network) that brings together diverse voices, organisations, and agendas to build shared learning in mental health safety. In November 2022, over 40 people across the three trusts, local authorities, police, and voluntary organisations attended the patient safety network which focused on learning from the trusts. Below is the key learning shared by trusts.
The programme actively engaged with experts by experience to improve inpatient care and reduce restrictive practice. We coproduced a video that features how communication can be improved in wards and how to make the wards become safer, calmer and more therapeutic environments. View the video.
To build good relationships with participating wards, we visited Goddington ward (Oxleas) and Churchill ward (Cygnet). The reflections of the HIN project manager, the practice development nurse of the ward and an Expert by Experience were captured in a blog here.
HEAL-D
African and Caribbean communities in the UK are three times more likely to develop type 2 diabetes than white Europeans, with onset ten years earlier, and poorer control following diagnosis. Healthy Eating and Active Lifestyles for Diabetes (HEAL-D) is a type 2 diabetes self-management programme for people of African and Caribbean heritage, which was designed to help tackle this.
HEAL-D was developed by researchers at King’s College London using co-production to ensure it reflected the needs of the community and content was culturally sensitive. The Health Innovation Network has supported south London delivery of HEAL-D and through the National Insights Prioritisation Programme.
The programme uses evidence-based type 2 diabetes guidelines for diet and lifestyle management and is underpinned by robust behaviour change theory. HEAL-D is designed to be fun and engaging, with participants able to bring a friend or family member along to support. It focuses on small, practical changes with discussions about relevant cultural foods and other aspects of diabetes which can help participants manage symptoms.
Post-programme evaluation suggests a reduction in PAID 5 score following attendance (indicating reduced diabetes-related emotional distress (diabetes distress)). Participants also report weight loss. Feedback about the course is largely positive with ‘strongly agree’ as the most common answer for all evaluation questions including ‘I feel motivated to follow HEAL-D advice’, ‘HEAL-D has helped me feel supported in living with diabetes’ and ‘HEAL-D has helped me learn to manage my diabetes’.
“I’m glad the doctors sent me to you, I was down and depressed. It helped lift me up.”
"[HEAL-D was a] call to make me take longer walks and enjoy the walks and cut back on the carbohydrates and eat more vegetables...I've actually lost weight."

Care Home Pioneers
supporting care home managers

This year marked the fourth year of our collaboration with My Home Life England, delivering a leadership development programme to Care Home managers across south London. The programme was generously funded by NHS England (London), South West London ICB, the London Borough of Bromley and the London Borough of Lambeth.
Thirty six ‘Care Home Pioneers’ joined the programme this year, drawn widely from across south London. Their leadership journey started with a series of workshops where they focused on how they managed themselves as leaders, how they lead others, and how they lead change. Subsequent Action Learning Sets gave the opportunity for the Pioneers to support each other and discuss workplace challenges.
Having learnt the fundamentals of quality improvement in a workshop delivered by the HIN team, Pioneers received mentoring from HIN staff to deliver an improvement project in their home. Projects were varied and included improvements in dementia care, and imaginative approaches to encourage residents to eat and drink well.
The programme culminated with a celebration day held in December, where the Pioneers spoke about the benefits of the programme and were able to showcase their quality improvement posters to funders.
A fifth cohort of the programme runs from April to December 2023, again generously funded by NHS and Local Authority partners.
3Supporting innovators
DigitalHealth.London
Accelerator

In the nine-month net promoter score survey, 100 per cent of company respondents said they would repeat the programme and the NPS score for the programme was in the excellent category.
Read this article for more examples of achievement from cohort six and to view their end-of-year summery posters.
The DigitalHealth.London Accelerator programme has now delivered six cohorts, supporting 143 companies in total. The programme was selected as winner of Accelerator of the Year award at the UKBAA Angel Investment Awards 2022.
Babblevoice, a purpose-built telephony system, achieved a
50%
reduction in did-not-attends (DNAs)

Joy, a digital Social Prescribing platform, leads to a
20-30%
decrease in GP surgery attendance

SiSU Health delivers community digital health checks via medial device health stations and has completed
20-30%
health checks in the UK

Launchpad
The Launchpad is an eight-to-12 week programme for early-stage digital health companies that have a product or service in development or ready to launch with high potential to meet NHS and social care challenges. The Launchpad supports companies by providing access to knowledge sharing events that help them understand demand in order to bring the product or process to market. The programme provides up to 12 hours of support consisting of workshops, bespoke one-to-one guidance from DigitalHealth.London consultants and advice from key founding and strategic partners to bring rich and diverse expertise across healthcare innovation.
Cohort four of the Launchpad took place March-May 2022. It received 60 applications and of those, nine companies were selected to take part. Following a three-month programme of support, eight have now launched their products. In the end of programme survey, the net promoter score was in the great category.
Cohort five of the Launchpad took place January-March 2023 and received 53 applications and of those, 14 companies were chosen to take part. So far eight companies have launched their products bringing the running total of products launched through the programme to 34.
Horizon Fellowship
In 2022 DigitalHealth.London announced the launch of the Horizon Fellowship programme, delivered in partnership with CW Innovation (the flagship innovation programme run jointly by CW+ and Chelsea and Westminster Hospital NHS Foundation Trust). The Horizon Fellowship programme builds upon the existing DigitalHealth.London Digital Pioneer Fellowship, which has already supported a number of Chelsea and Westminster Hospital staff members working on digital transformation projects. The programme equips the Fellows with new skills and knowledge, inspires them by providing opportunities to hear about the art of the possible from others, and connects Fellows to like-minded peers and mentors.
This year the Horizon Fellowship supported 15 individuals with transformation project ideas to improve patient care. During the recruitment process, we worked with the CW Innovation team to ensure the Fellowship was socialised with people from a diverse set of departments and backgrounds.
The 2022/23 Horizon Fellows’ projects are estimated to impact over 13,000 patients over the year and the net promoter score for the programme is in the excellent category.

The cohort represented 17 different departments and 55 per cent identified as Black, Asian or from an ethnic minority communities.
Wider Innovation Support
We ran 146 innovation clinics, of which 34 were hosted by our mental health team.
In September 2022 we held a roundtable in partnership with the Association of British Healthtech Industries (ABHI) where we invited companies to help us gather insights on challenges and opportunities for the UK healthtech industry.
We also delivered a showcasing webinar on the use of the Organisation for the Review of Health and Care Apps (ORCHA) for our south London stakeholders, in partnership with Kent Surrey Sussex AHSN. Attendees heard from other NHS organisations who use ORCHA to select safe and quality-assured health and wellbeing apps.
Race Observatory
We were commissioned to gather insights into the use of equality impact assessment in the procurement and implementation of new treatments and disruptive digital and technologies and produce standards for any organization completing EIAs prior to commissioning or funding new innovations. This work was commissioned following the Observatory’s rapid review in 2021 of pulse oximeters and less accurate measurements for people with dark skin. We undertook a mixed-methods research study with industry and NHS organisations to identify good practice and contribute towards producing the standards.

Good Boost
The Good Boost project won a HIN Innovation Grant to pilot a personalised water-based fitness programme supporting patients with musculoskeletal (MSK) conditions. It was launched in Southwark in April 2021 and also piloted at Kingston Hospital. It was open to people with long-term MSK conditions, those recovering from joint replacement surgery and older people. It used Artificial Intelligence (AI) to tailor an exercise programme to individual health condition, fitness level and confidence in the water. After five months:
- two-thirds of participants reported an improvement in their health;
- almost a quarter reported improvements in their functional capacity; and,
- more than a fifth reported a reduction in pain levels.
Graduates into Health –
Graduate Digital Data and Technology (DDaT) Scheme
The HIN were awarded the NHS England (NHSE) contract to deliver the NHS Graduate Digital, Data and Technology (DDaT) Scheme through to March 2025, worth £1,275,600. The contract is to continue delivery of the renowned graduate programme, which we have delivered since 2018, as well as work with NHSE to support trusts with their Electronic Patient Record (EPR) digital transformation programmes.
The Frontline Digitisation Programme is an ambitious national programme to support all Trusts to implement EPRs that meet the Minimum Digital Foundations (MDF) by March 2025. As part of the overall support package, NHSE is providing funds to the least digitally mature trusts to enable them to commission the Graduates DDaT Scheme to provide part of their EPR staffing structure. In 2022/2023 the scheme has been commissioned by a significant number of new Trusts to recruit 79 DDaT graduates at bands 5 and 6 in EPR support roles such as robotics, data analytics, configuration analysts, project support, software development, cyber security and networking.
Through this EPR-focused support, alongside the business as usual roles we recruit, the Graduate Scheme is scaling up its provision to recruit and support up to 200 graduates per year. The scheme is transforming its operations to enable continued support to an increased number of graduates on programme while continuing to deliver the flagship Graduate DDaT Scheme the system has relied on, to fast-track tomorrow’s talent, into the NHS today.
Key Achievements
graduates supported on programme in 2022 -2023
Electronic Patient Record (EPR) graduate roles commissioned over 16 trusts in 2022 – 2023
Business as Usual (BAU) graduate roles commissioned over 16 trusts in 2022 – 2023
EPR graduate progression rates:
-
- 30 graduates trained and supported in 2022/2023
- 10% band 6 graduates remained at band 6
- 83% band 6 graduates progressed to band 7
- 7% of band 6 progressed to band 8a
Of 122 graduates on the programme:
-
- 24% graduated with a Masters or PHD
- 24% obtained a 1st class degree
- 34% obtained a 2:1 degree
graduates selected for the scheme at assessment centre, since 2018
graduates successful in moving into band 6/7/8a roles through the scheme, since 2018
graduate retention rate, since 2018
Virtual Wards and Remote Monitoring Technology work for NHSE London
In 2022, NHS England dedicated £450 million towards establishing 40-50 virtual ward ‘beds’ per 100,000 population by October 2023. The national programme defines virtual wards as a safe and efficient alternative to NHS bedded care, supporting patients who would otherwise be in hospital to receive the acute care, monitoring and support they need in the place they call home. While some national guidelines have been issued, including mandating respiratory and frailty pathways, much of the responsibility around design and implementation has been left to local systems and there is a lack of consensus about the optimal approach.
In response to the range of technologies in use and market being in growth stage, we produced a guide specification to support London Integrated Care Boards (ICBs) procuring virtual ward technology. These materials have been used to support procurement processes at two London ICBs, providing content for presentations to committees and validating local approaches to procurement. This should help increase standardisation and reduce variation in care for patients across the region. The 2022 review of the market showed variation in technology use across the capital.
On behalf of the London region the HIN has delivered a series of projects to:
- Understand the use of remote monitoring technologies;
- Assess the maturity of the market;
- Support ICB procurement through the development of a technical guide; and,
- Providing recommendations on developmental partnerships with suppliers.
The first project involved a horizon scan, gathering lessons learned from early adopters of remote monitoring across London and providing market analysis around solutions available, including mapping solutions according to the level of care required, analysis of interoperability and functionality.

The most recent project produced recommendations around procuring partnerships with industry to co-develop novel remote monitoring solutions. This aims to accelerate the development of technologies that can best support the needs of patients on virtual wards and the staff providing their care. Two procurement roundtables were held in January 2023, with 20 experts from senior NHS, procurement and industry roles attending to advise on best practice for procurement and partnerships with remote monitoring suppliers. A report summarising the roundtable and a final report have been published.
SELCA Personalised Care Market Review Summary
The NHS Long Term Plan states that every person with cancer should have access to health and wellbeing information and support before, during and after their treatment, making up one of the four personalised care interventions within the Plan. To help clarify the digital component of this aim, South East London Cancer Alliance (and later, the three other London-based Cancer Alliances) sought to understand the market for personalised care platforms applicable to cancer, enabling person-centred decision making and improving patient management for clinicians.
The HIN were commissioned to deliver a project with three core purposes:
Consolidate market information
- Enable clinical and project staff to navigate the market.
- Better manage engagements with companies that approach them.
Assess the current market
- Identify and compare solutions that deliver personalised care in the context of cancer services. This work explored the capabilities and commercial offerings of platforms and standalone solutions (eg apps) which supported service delivery and patient self-management.
Inform future personalised care module development
- Conduct market engagement and explore the adoption of similar technologies in other parts of the health system, ensuring proposed solutions were fit for purpose.
Recommendations were provided for future market engagement, selection and implementation. These were further were categorised into provider, system, and patient perspectives to provide insights specific to these key stakeholders.
The report findings have been presented to all London Cancer Alliances and their respective personalised care programme boards. We have been asked to present the findings of this report at the Oncology Professional Care 2023 conference.
As a result of our work, one of the included solutions (ONKO) was selected for a pilot in the Breast and Lung Cancer Pathways at Lewisham and Greenwich NHS Trust.
London Digital First Primary Care Automation Grants of up to £65k were awarded to projects across London to pilot automation solutions in primary care.
Automation refers to the design and implementation of technologies to provide services with minimal human involvement. Automating high-volume, repetitive, rule-based tasks can improve productivity, efficiency, reliability, compliance, speed and accuracy, colleague morale, and integration between people and process. This can help free up clinical and administrative staff so they can focus on securing the best possible outcomes for patients.
Following the production of an Automation in Primary Care Review report in 2021/22 for the London Digital First Primary Care team, the HIN was asked to administer a Primary Care Automation Grants programme on behalf of the regional office. Grant applications were assessed upon the scope, scale, impact, sustainability, and opportunities for spread and adoption of their projects. Over £600,000 was awarded across 11 innovative primary care automation projects across London involving automation solutions addressing clinical and/or administrative challenges. Pilots are being monitored over a 12-months period against agreed metrics, before being evaluated. The projects are due to complete in Autumn 2023.
Over £600,000 was allocated across 11 innovative primary care projects in London.
“Primary care faces an ever-increasing workload. It is exciting to see these automation pilots provide hope for a range of solutions to tackle this workload with improved outcomes for both staff and patients. It might not be long before we look back and wonder how we ever managed without some of these automation solutions” - Dr Shanker Vijay London Region GP Clinical Lead Digital First Programme, NHS England
“The grants programme provides a unique opportunity for us to pilot a variety of innovative automation solutions that can transform the way practices manage their workload. We hope that through this work patient care and staff morale will be improved by automated processes freeing up both clinical and administrative staff from some of the most time-consuming and repetitive tasks they currently undertake." - Matt Nye, Director, London Digital First Programme
4Evaluating innovation
South West London virtual ward evaluation
As part of a series of evaluations looking at the use of remote monitoring in supporting the management of long-term conditions across different clinical pathways in London, the HIN carried an evaluation of three virtual wards in south west London: Sutton, Kingston and Richmond, and Croydon.

Sutton Virtual Ward
- Launched in February 2021;
- Primary care led, with Sutton Health and Care delivering the service.

Croydon Virtual Ward
- Piloted in July 2020, and fully deployed in September 2020;
- Acute-led, community-delivered, currently sits with Croydon Health Services NHS Trust.

Kingston and Richmond Virtual Ward
- Soft launch in December 2021;
- Acute-led model of care, currently sits with Kingston Hospital NHS Foundation Trust.
We found that the three virtual ward models, although set up differently, were successful at treating patients safely and comfortably at home, through a combination of remote monitoring, telephone calls, and home visits.
Key findings include:
- High levels of adherence to the technology: for instance, the vast majority (98 per cent) of Croydon patients were able to engage with the technology;
- Low rated of hospital readmission: data on hospital admissions 30 days after discharge from the Kingston and Richmond virtual ward showed that only seven patient admissions (17 per cent) had been admitted to hospital in the 30 days after being discharged from the service;
- Patients and their carers felt they received the same standard of care as they would in a hospital environment;
- Clinical virtual ward staff reported positive working experiences.
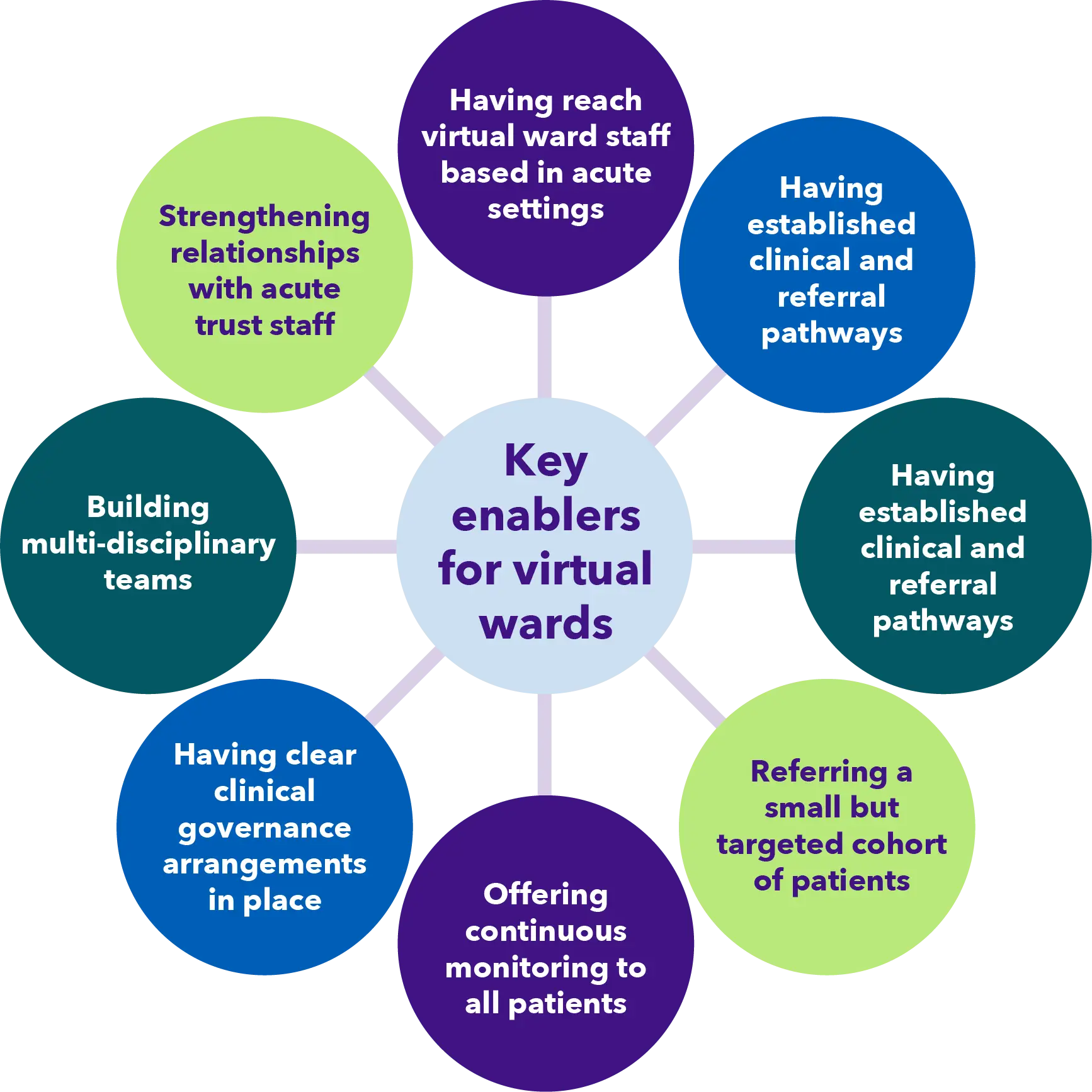
Further evidence is needed however to understand the full impact of virtual ward services on healthcare utilisation in south west London. A number of key enablers for virtual wards to prevent admissions into acute hospital beds, or supporting early discharge out of hospital were identified.
A few key stats:
Kingston and Richmond
- Length of stay ranged from one to 29 days, with a median average length of stay on the virtual ward of 13 days;
- Over a quarter of patients wore their device for 60 per cent or more of their time on the ward, giving them complete adherence to the technology;
- Data on hospital admissions 30 days after discharge from the virtual ward showed that seven patient admissions (17 per cent) had been admitted to hospital in the 30 days after being discharged from the virtual ward.
Sutton
- The average (median) length of stay on the virtual ward was 10 days;
- The majority of patient admissions were discharged back to their usual place of residence (74 per cent), with just over a quarter (26 per cent) being admitted to an acute hospital.
Croydon
- The average (median) length of stay on the ward was 7 days.
- A large proportion of virtual ward admissions were for acute episodes (60%).
- The vast majority (98%) of patient admissions were able to engage with the technology.
- The discharge outcomes from the Croydon virtual ward showed that 81% of patient admissions remained at home until they were discharged from the ward. This included 72% that remained at home with only remote access to healthcare, and a further 9% who also remained at home but received a home visit during their time on the virtual ward.
London NHS Mental Health Crisis Hubs Evaluation
In 2022, NHSE London commissioned the HIN to complete an evaluation to gain an understanding of the different mental health crisis hub models that are in operation and their potential impact at a service user, carer, practitioner, and service-level within London.
Four mental health trusts in London were included in the evaluation:
- Two that provides a mental health crisis hub that allows direct access to service users who are in a mental health crisis;
- One that requires service users to attend the emergency department to be referred to the crisis hub;
- One that was a Psychiatric Liaison Service.
Although it is relatively early in the lifetime of the two hubs that allow direct access, the evaluation was able to evidence that both these hubs:
- Provide a timely service that enables service users to be seen on arrival by a mental health professional;
- Have a growing proportion of service users that go directly to the hub and are evidencing that service users who have attended these hubs once, are more likely to self-refer if they need to attend again.
The majority of service users who provided feedback on experience of these hubs said that they felt safe, had privacy, and were treated with kindness and respect by staff within the hubs who had a good understanding of mental health. There was however significant service user, staff, and stakeholder feedback on where improvements could be made for all the hubs included in this evaluation. Read the full report and plain English summary.
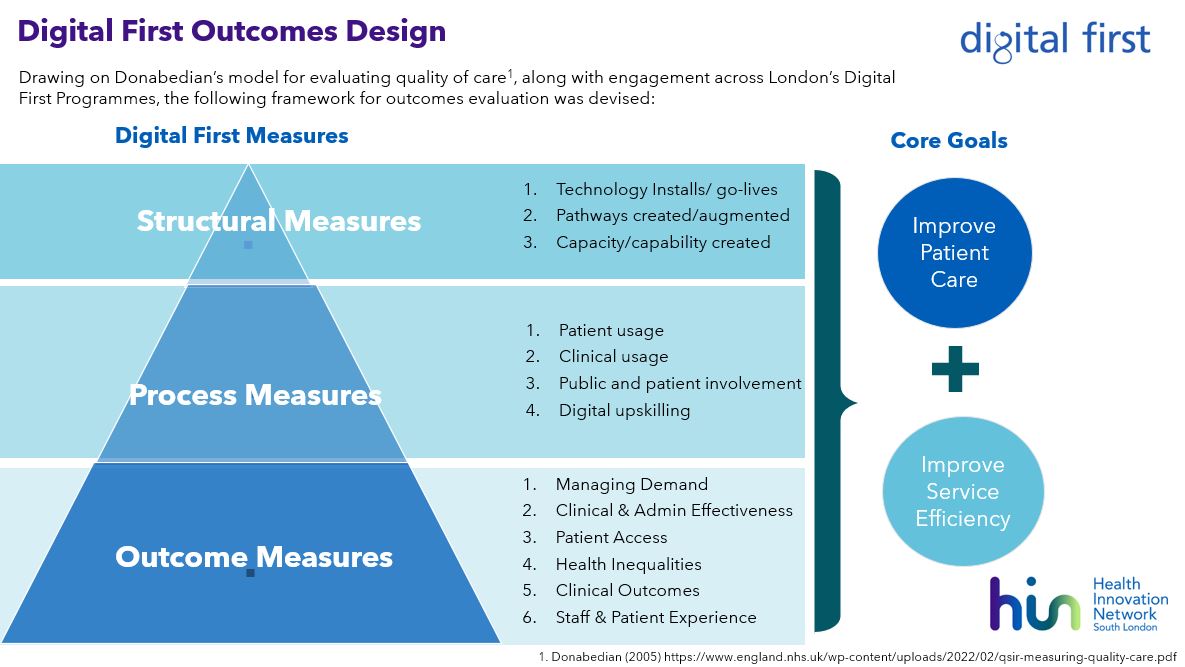
Digital outcomes framework
To demonstrate the impact of all initiatives within the Digital First Programme, the NHSE London Regional Team commissioned the HIN to create a Digital First Outcomes Framework to be used by local Digital First Teams to capture, review and track their own local outcomes relating to the programme.
To support the adoption of the Outcomes Framework a series of materials were developed, as shown on the right.
These materials are available to download via FutureNHS.
London Digital First Outcomes Framework Pro-forma
Excel version of London Digital First Outcomes Pro-forma
Useful Data Sources for London Digital First Outcomes
Outcomes Tracker
The framework was created through:
- Research on existing outcomes frameworks and evaluation models, and existing outcomes collection models being used by ICB Digital First teams;
- Iterative and collaborative engagement and needs articulation with each ICB Digital First team to agree on the framework, its use, and a set of outcome measures to be applied;
- Testing of the framework and supporting materials with selected projects across the Digital First programme of work;
- Socialisation of approach by delivery of ICB level workshops to provide guidance on how to use the framework and how it can be tailored to local needs.
Framework
DigitalHealth.London Generator
The Generator has facilitated 43 new research collaborations between digital health companies and researchers
Evidence Generation Bootcamp
Thirteen companies were chosen to take part in the programme and were given the opportunity to attend a series of virtual events including educational workshops, webinars and pitching sessions.
The Bootcamp programme received a net promoter score in the "excellent" category and the weekly workshops received consistently positive feedback, with an average of 98 per cent giving a score of either four or five out of five when asked how useful they found each session.
5Finance and People
People section
(including health and wellbeing and anti-racism)
The HIN has had a particular focus on anti-racism this year. We have held a series of workshops with staff to enhance confidence and capability in discussing race and tackling racism and health inequalities. We now have anti-racism champions in each HIN team and have developed a specific organisation goal and associated mission statement. Our goal is to be an actively anti-racist organisation with a mission statement: overcoming racial inequality in our workplace and community.
Our new Involvement Strategy included the aim of ensuring that the voice of people who live and work in south London is embedded in the selection of national innovation priority programmes, and their local translation. Two lived experience partners have been recruited and started work at the HIN in February 2023. Part of their remit is to link us with wider communities of people living in south London so there is influence from people not usually involved in our project work.


Overall financial position
- £’000
- Income
- 9,714
- Expenditure
- 9,497
- Surplus
- 217
Funding sources
- Income
- £’000
- NHS England
- 5,088
- Patient Safety Collaborative
- 495
- Office of Life Sciences
- 867
- South East London ICB
- 740
- South West London ICB
- 208
- NHS Trusts
- 1,114
- Other NHS organisations
- 74
- AHSNs
- 146
- Third Sector
- 162
- Companies
- 130
- Local Government
- 93
- Government
- 480
- Universities
- 117
- Total
- 9,714
Expenditure
- Expenditure
- £’000
- PayNon-PayTotal
- Central Costs
-
8208941,714
- Corporate Support
-
638-638
- Communications
-
41356469
- CVD Prevention
-
33610346
- Diabetes
-
31660376
- Patient Safety & Experience
-
6624791,141
- Healthy Ageing
-
31452376
- Mental Health
-
32056376
- Accelerated Access Collaborative
-
2392241
- Muscoloskeletal (MSK)
-
16622
- Innovation
-
18811199
- Graduates into Health
-
386398784
- Digital Transformation & Technology
-
373492865
- Evaluation and Informatics
-
856133989
- DigitalHealth.London Accelerator
-
837134971
- Total
-
6,7142,7839,497
Pay gap
We are committed to improving diversity, inclusion and equality. In the interests of transparency we publish data annually relating to the gender and ethnicity pay gap among staff at the HIN. The latest available data for 2022/23 is below.
As a relatively small organisation, caution should be exercised when interpreting the data, particularly where it is further broken down, for example when data is split into pay grades.
We recognise that our staff do not collectively represent the diversity of our south London population, which is why we are working to avoid recruitment bias and ensure we are an inclusive and welcoming employer. Externally, we continue to prioritise the reduction of health inequalities in all our projects and encourage our partners to do the same.
Gender
Mean hourly pay: men 18 per cent higher than women. In 2021/22 men were 27 per cent higher than women.
Median hourly pay: men eight per cent higher than women. In 2021/22 men were 14 per cent higher than women.
Ethnicity
Mean hourly pay: those who identify as white four per cent higher than those who identify as being from an ethnic minority. In 2021/22 the mean hourly rate for those who identify as being from an ethnic minority was seven per cent higher than those who identify as white.
Median hourly pay: those who identify as white eight per cent higher than those who identify as being from an ethnic minority. In 2021/22 the mean hourly rate for those who identify as white was 11 per cent higher than those who identify as being from an ethnic minority.
This is driven by salaries across a range of staff roles and working patterns.
Breakdown of diversity by band
| Band | Gender | Ethnicity | ||||||||
| Total | Men | Women | Total | White | Ethnic minority | |||||
| 4 | 7 | 1 | 14% | 6 | 86% | 6 | 3 | 50% | 3 | 50% |
| 5 | 10 | 3 | 30% | 7 | 70% | 10 | 5 | 50% | 5 | 50% |
| 6 | 4 | 1 | 25% | 3 | 75% | 3 | 3 | 100% | 0 | 0% |
| 7 | 21 | 6 | 29% | 15 | 71% | 20 | 12 | 60% | 8 | 40% |
| 8a | 22 | 7 | 32% | 15 | 68% | 21 | 15 | 71% | 6 | 29% |
| 8b | 8 | 3 | 38% | 5 | 62% | 7 | 7 | 100% | 0 | 0% |
| 8c | 6 | 2 | 33% | 4 | 67% | 6 | 5 | 83% | 1 | 17% |
| 8d | 7 | 2 | 29% | 5 | 71% | 7 | 6 | 86% | 1 | 14% |
| Very Senior Manager (VSM) | 6 | 3 | 50% | 3 | 50% | 5 | 3 | 60% | 2 | 40% |
| Clinical Director (part-time, various contracts) | 7 | 4 | 57% | 3 | 43% | 6 | 3 | 50% | 3 | 50% |
| Total | 98 | 32 | 33% | 66 | 67% | 91* | 62 | 68% | 29 | 32% |