Andy Scott-Lee recently joined our Mental Health team, having spent most of his career with front-line mental health roles. We speak to him about his reflections on his first few months at the Health Innovation Network and what his experiences have made him think about how we could protect and improve the mental health of our nation.
Every week, so it seems, a new worry is added to the list of issues affecting society. Between the housing crisis, the climate crisis, and the cost-of-living crisis, there seem to be more factors than ever making life difficult for ordinary people.
In a world where everyone is affected by these issues differently, where do we start when it comes to finding common ground for improving our nation’s mental health and wellbeing?
In my opinion, it all begins with looking out for the people looking after our mental health.
Most clinical teams working in mental health are under significant pressure at the moment. I think awareness of those stresses probably peaked during Covid-19, where we saw a significant increase in mental health issues experienced by NHS staff, but it’s so important that we don’t slip into thinking those operational pressures have gone away.
People working in the NHS need to feel they are valued and that they and their services are supported by their organisation to do the job they were trained to do. I've worked on the front lines of mental health, and so often have found that the times where I delivered the best care were when I felt my health and wellbeing were being prioritised.
To be authentic and consistent in my care for others, I needed to first feel good about myself.
Making time to change our culture
Improving the way we look after our workforce is a responsibility for everyone working in mental health.
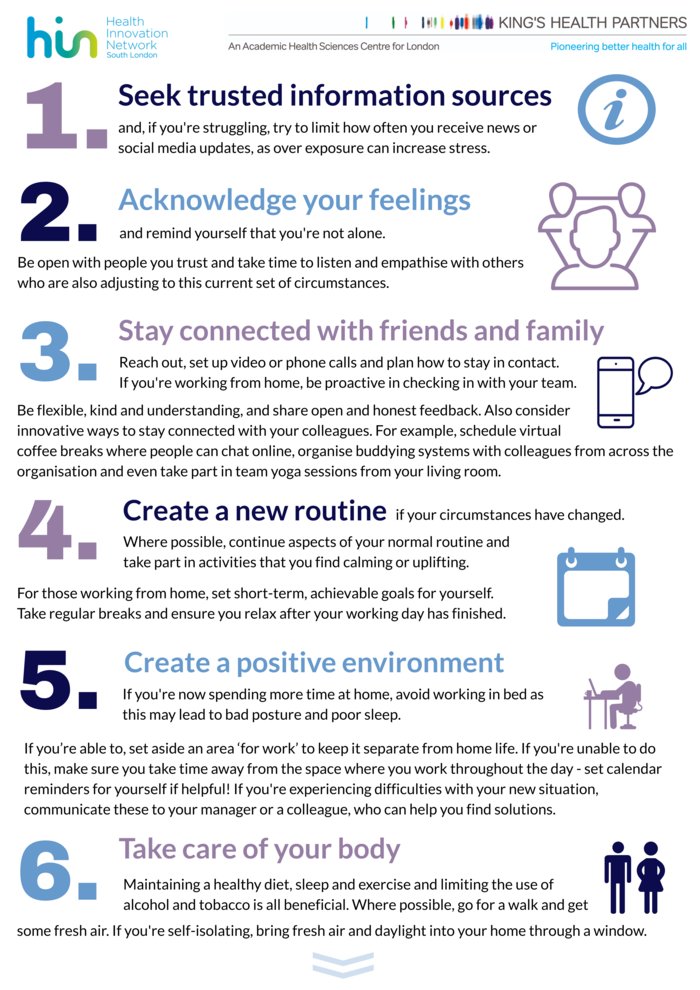
Many mental health professionals already take a mindful approach to their own wellbeing, and I feel this is something we should continue to encourage. Certainly, the mantra of "be gentle on yourself" was something that I repeated to myself when treating many of my patients with trauma, and there is a wealth of insight and guidance on effective self-compassion dating back as far as Buddha. But self-help is only a part of the solution.
One of the biggest things I’ve noticed since joining the HIN is that wellbeing isn’t just listed as an “organisational priority” – it is something that everyone actually invests time and effort into.
Finding everyone represented in health and wellbeing conversations has been a relieving and refreshing experience. At all levels, it is acknowledged that the time and effort that goes into improving our wellbeing is reflected in the quality of the work that we do. Dedicated wellbeing champions lead the way, and it is great to see staff from all backgrounds and seniorities consistently taking advantage of activities designed to improve our physical and mental health.
Of course, the HIN does have significant organisational differences to a Trust providing clinical care. But I think the essence of what we have here – senior leadership buy-in, dedicated champions and advocacy across the organisation for wellbeing as a priority – could be applied anywhere.
Practical action, not policies
Health and wellbeing isn’t a new topic within the NHS; NHS England’s People Plan from 2020 is full of sound thinking on the issue.
But despite “islands of improvement” we haven’t made enough progress as a system, and perhaps we’ve fallen into the trap of talking too much and acting too little.
So my challenge to people working in mental health is this – what can you do to improve the wellbeing of our workforce, and in turn improve the care that we provide?
Can you find a way to reduce the workload of someone so that their “wellbeing champion” objective becomes part of their core responsibilities rather than an add-on to do in their personal time?
Can you be the senior leader who always makes time to attend a wellbeing walk or other activity?
Can you be the person who takes the initiative to learn from what’s working elsewhere?
I believe you can.