Evidence-based audit and feedback
August 15, 2022In response to the nationally commissioned Medicines Safety Improvement Programme (MedSIP), the Health Innovation Network has developed a local programme aiming to reduce opioid-related harm to patients experiencing chronic pain (non-cancer related).
The Patient Safety Collaboratives (PSCs) are working with at least 50% of Integrated Care Boards (ICBs) across England, will collectively achieve the ambition to improve care for people with persistent (chronic, non-cancer) pain by reducing opioid analgesic use by the end of March 2025.
To support practices, they were provided with a resource pack signposting resources to support staff in general practice to review patients prescribed high-risk opioids (e.g. patients on opioids for more than 12 weeks for chronic pain and those prescribed high doses). The approach was modelled on a successful campaign undertaken by the West Yorkshire Research and Development team and their support enabled the production of opioid prescribing reports.
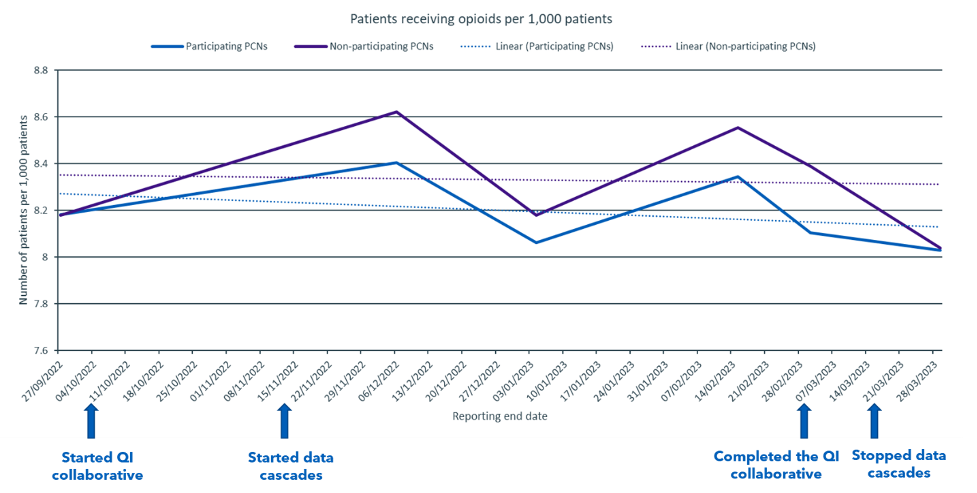
Monthly reports were cascaded through medicines optimisation leads to general practices between November 2022 to March 2023. The reports were based on NHS BSA Opioid Prescribing Comparators dashboard, to help practices understand their own opioid prescribing trends and to increase awareness of the dashboard. The objective was to encourage a reduction in inappropriate prescribing of high-risk opioid prescribing in chronic pain.
The graph below highlights the impact of both the QI collaborative and evidence-based audit and feedback across general practices in south London.