Event: Empowering Patients to Self-Manage

Our interactive webinar “Modernising Primary Care Telephony” took place on Wednesday 2 March, 12:30-14:00.
The webinar showcased telephony innovations, highlighting the potential for modern telephony to improve communication in primary care across London.
Presented by the Health Innovation Network in collaboration with the NHS England Digital First Programme London, we looked at how updating traditional telephone systems can improve interactions with patients and support PCN development, flexible and remote working and help streamline service delivery.
This event updated primary care staff about emerging national plans around primary care telephony and built on previous work undertaken in this area through the Digital First Programme and learning from ongoing projects. The event also showcased several products on the market, helping primary care staff understand the breath and depth of functionality that can transform primary care processes.
In addition, the HIN has produced a commissioning guide on Modernising Primary Care Telephony which is now available for download from the Health Innovation Network’s website. This report was commissioned by Our Healthier South East London ICS (OHSEL)through the Digital First Programme and delivered by the Health Innovation Network, the Academic Health Science Network for South London.
You can access the event pack and running order here, and the slide deck here.
Video Running Order
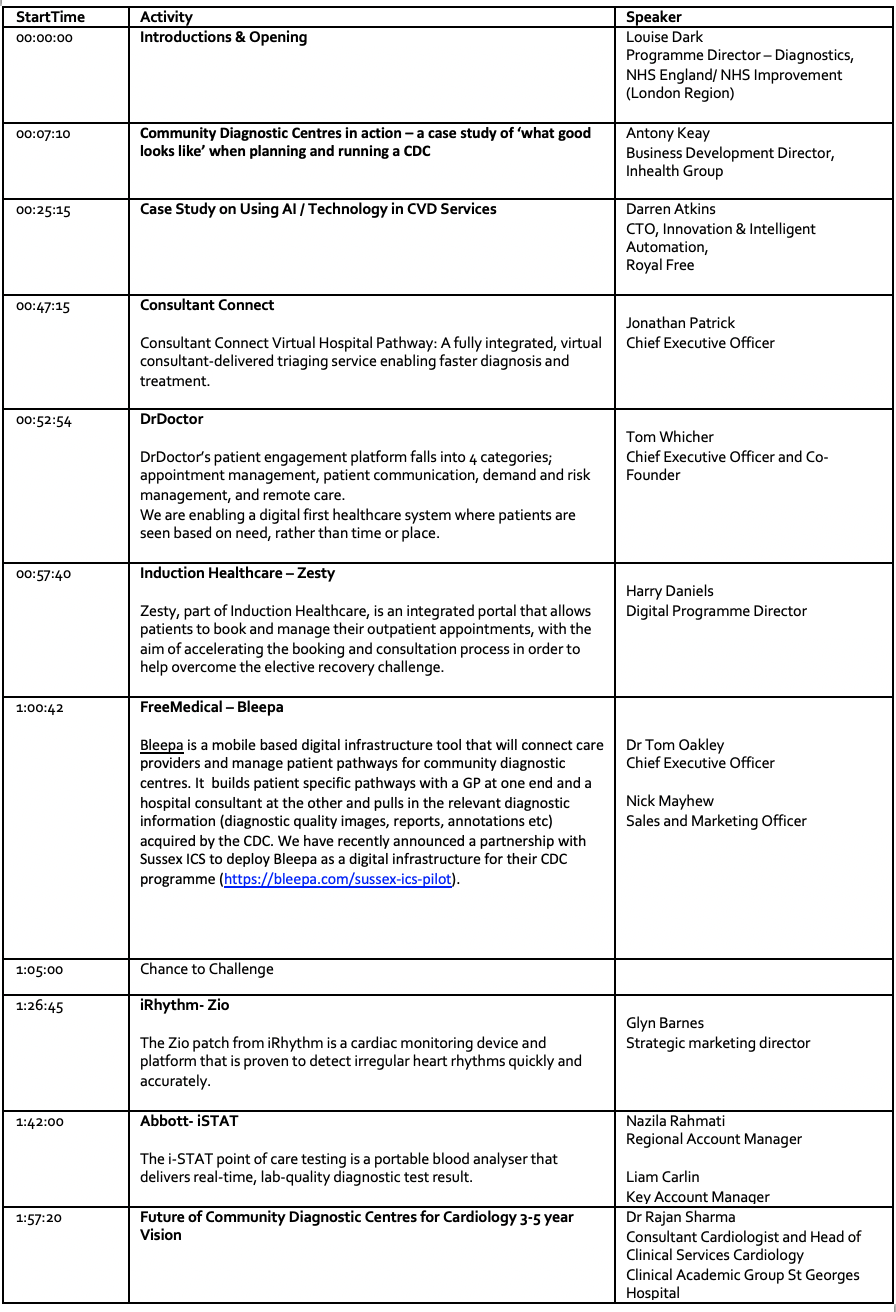
| Start time | Topic | Presenter |
| 00:00:00 | Introduction from Chair/
Health Innovation Network
|
Denis Duignan
Head of Digital Transformation & Technology Health Innovation Network |
| 00:04:50 | Presentation:
A London region perspective around the opportunities of modern telephony in primary care. |
Matt Nye
Regional Director for Digital First Programmes NHS England (London) |
| 00:09:57 | Five 2-minute pitches*
|
Babble Ltd
Product: Babblevoice Antoine Lever Director EVAD Think Healthcare Product: Think Healthcare Solution Mike Smyth Think Healthcare Team Leader Exponential-e Product: UC-One Tim Gilliatt Public Sector Account Manager Gamma Product: Horizon, the modern Primary Care telephony choice Amy Black Business Development Executive Premier Choice Group Product: Premier Patient Line James Gargaro Sales Manager |
| 00:24:31 | Presentation:
Taking an ICS wide approach to primary care telephony |
Brian Stennett
NWL GP Telephony Lead, Digital First North West London CCG |
| 00:34:07 | Four 2-minute pitches* | Voice Connect Ltd
Product: Cloud Based Patient Partner with Automated Telephony Repeat Prescriptions Review and Ordering Service Paul Trayler Sales Director VTSL Limited Product: GP Cloud Voice Rob Walton CEO X-on Product: Surgery Connect Desktop App Paul Bensley Director Yo Telecom Product: Bespoke Phone System Daniel Mills Senior Consultant |
| 00:41:02 | Presentation:
Advanced Telephony National Update |
Nikki Hinchley
Head of GPIT Transformation, Digital Primary Care NHS Transformation Directorate / NHS England & NHS Improvement |
| 00:47:27 | Panel discussion and Q&A session | Speakers and Chair to take questions from the audience |
| 01:16:13 | Closing remarks | Chair |
| * The Health Innovation Network and NHS England do not endorse or recommend any of the commercial innovations showcased at this Innovation Exchange event. The innovations referred to at the event are not preferred suppliers and there are other solutions that can support the challenges identified. This event is intended to inspire people as to how innovations can support health system problems, rather than endorse any specific solutions, with the sole intended purpose to be for guidance only. |