Download the report
Read the full report to learn more about the project's aims to improve mental health and wellbeing outcomes for people who have participated in pulmonary rehabilitation.
Download
More than 15 million people in the UK live with one or more Long Term Condition (LTC) and over 4 million of these individuals also experience mental health problems. A significant proportion of these people are living with poor respiratory health such as asthma and chronic obstructive pulmonary disease (COPD). Pulmonary rehabilitation (PR) is an exercise and education programme designed for people with lung disease or respiratory conditions, who experience symptoms of breathlessness. PR can also be used as a tool to improve mental health and wellbeing, however, there is not always a clear pathway within PR to access mental health support, and non-attendance can be a result of depression and other mental health issues.
South East London’s Integrated Care System and King’s Health Partners (KHP) have established the South East London Coalition for Better Health and Equity, a programme focused on enhancing population health outcomes, addressing disparities, and promoting equitable access to healthcare services for communities across South East London. The programmes approach includes:
1. Embedding the Vital 5 interventions, which are the five risk factors that have a major impact on health: blood pressure, obesity, mental health, smoking status, and alcohol intake;
2. Delivering better mental health outcomes for people with LTCs.
The Health Innovation Network (HIN) South London were commissioned as a co-design partner to work with KHP to plan, deliver, and report on a co-design project focusing on improving access to mental health and wellbeing support for patients with LTCs. This project aimed to improve mental health and wellbeing outcomes for people who are eligible for or have participated in PR.
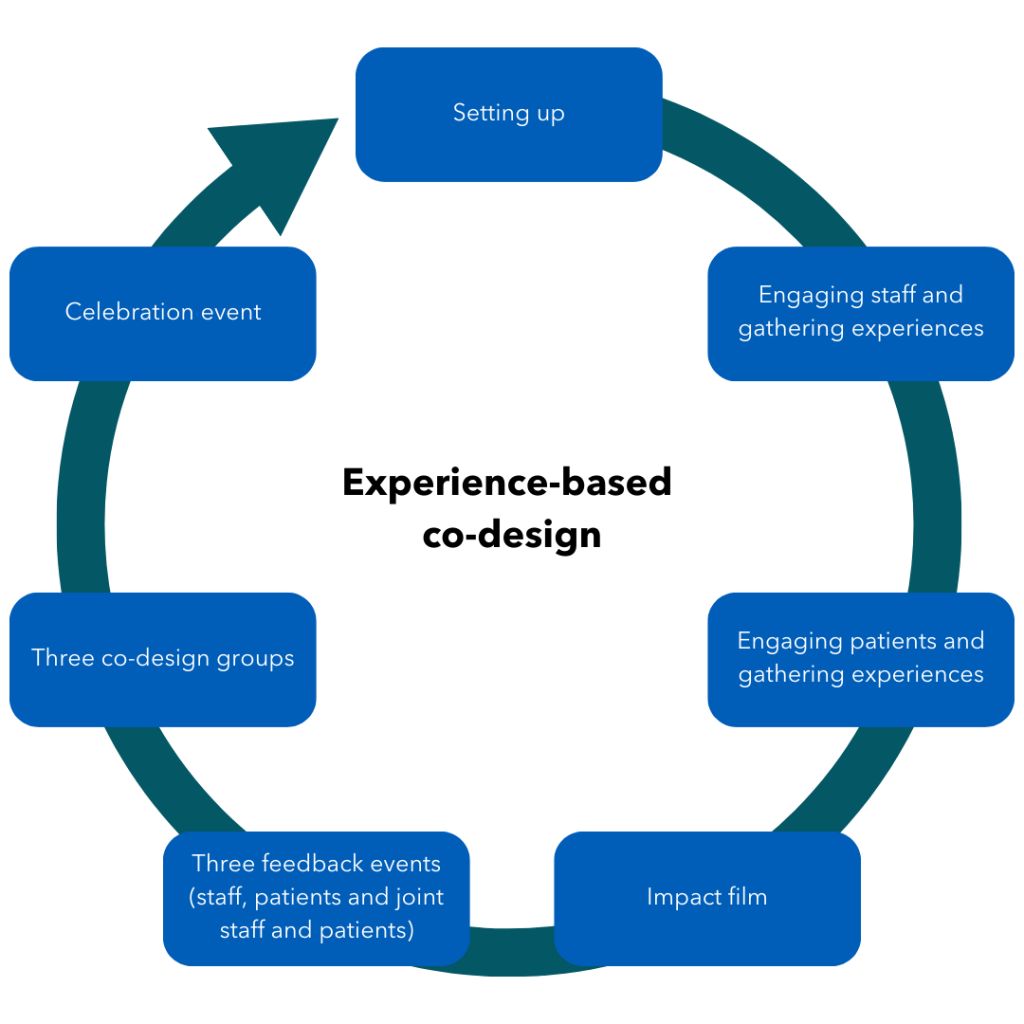
A methodology called experience-based co-design (EBCD) was used for this project. This method, developed by the Point of Care Foundation, is an evidence-based approach which involves collecting and sharing insights to build understanding and develop solutions. An impact film is created using clips from patient interviews, which reflects participants’ stories of service and amplifies impactful moments. These experiences provide a platform for patients and staff to co-design realistic recommendations in a series of workshops, ending with a celebration event.
9 patients from five of the six SEL boroughs who had attended PR (including one patient who had been identified as high risk of not completing PR) took part in the interviews, workshops and co-design events;
7 staff were also interviewed with representation from six organisations and roles in PR services, talking therapies, primary care, and health inclusion;
12 staff members attended the feedback events and co-design workshops, representing eight organisations.
People who had attended PR gave equal weighting to positive elements and barriers they experienced. Highlights of these findings included:
Although not included in all PR sessions, where available the social aspect of pulmonary rehabilitation was greatly valued, supporting wellbeing of attendees in an informal way through peer support.
Education sessions about mental health and the interaction between LTCs and mental health and wellbeing as part of PR were highlighted for being informative, helpful and reassuring.
People did not know what to expect of PR, and as a group reflected that educational material and information at the point of referral was not consistent. This view was supported by the staff group.
The recommendations came directly from the co-design process, using patient perspectives as well as staff experience.
Integration of services and roles known to support people’s mental health throughout the pathway.
PR services should provide consistent and accessible information to participants.
Participants’ mental health and wellbeing should be screened (using validated tools) in a consistent way.
Language and terminology should be helpful in raising people’s understanding and awareness. For example the terms ‘mental health’, ‘mental illness’ and ‘wellbeing’ should be adopted and used in tandem.
Staff and volunteers should be supported to gain appropriate skills and use available tools to help participants.
PR services should provide an element of informal peer or social support.
Participants who complete the programme should be given information on where and how to access support for both physical and mental wellbeing.
PR services should take a quality improvement approach to understanding and addressing the reasons why participants do not start or drop-out after one or two sessions.
Read the full report to learn more about the project's aims to improve mental health and wellbeing outcomes for people who have participated in pulmonary rehabilitation.
Download