Blog
Post Title
In this edition, we caught up with Gabe Jones, Consultant in Emergency Medicine at St George’s Hospital and Director of Patientcheck.in which allows patients to provide simple clerking information and see their accurate waiting time on their smartphone, while they wait.
Tell us about your innovation in a sentence
Patientcheck.in allows patients to check in to the Emergency Department (ED) and tell staff why they are attending – using their own words and a smartphone.
What was the ‘lightbulb’ moment?
Basically, it became obvious almost every aspect of the modern world now works like this. It just makes the current process in most EDs seem ridiculous (I’m sure most patients will agree).
Are there any exciting things in the pipeline for Patientcheck.in’?
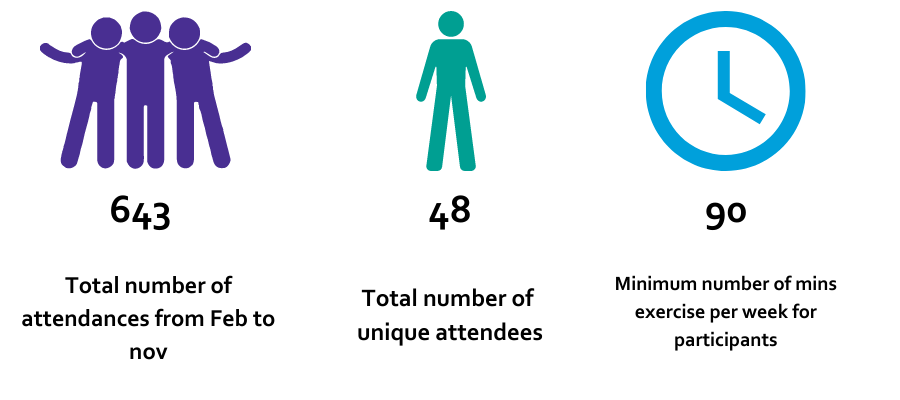
Patientcheck.in has been realised on the back of a grant from the Health Innovation Network. Without this support it’s hard to see how we would have managed to get off the ground. Having developed and trialled patientcheck.in with over 30,000 patients we are looking forward to sharing the solution when we launch later this year.
What three bits of advice would you give budding innovators?
- Speak to as many people as you can. You won’t get very far unless you have convinced at least a few people to lend their support.
- Don’t take no for an answer. The reality of the NHS is that everyone has a million things do to and almost no time or money to do them. It’s not Google.
- Plan your next three moves. It’s easy to lose momentum and get bogged down.
What’s been your toughest obstacle?
Navigating the seemingly never-ending complexity of the NHS. It’s like peeling an onion, one layer at a time. When you think you are getting somewhere, you suddenly realise that not only are there another ten layers, but there is a whole sack of onions you didn’t even know about. For example, simultaneously working your way through governance, compliance, data protection and ethics with all the relevant bodies requires both patience and persistence.
What’s been your innovator journey highlight?
The whole journey has been fascinating. I’ve met a lot of interesting people and I’ve learnt lots of new skills, as well as a better understanding of the logistics and business side of healthcare. It’s a great feeling when you see your idea actually being used and making someone’s life a bit easier.
Best part of your job now?
Having the opportunity to improve patient care in a meaningful way.
If you were in charge of the NHS and care system, what’s the one thing you’d do to speed up health innovation?
Streamline and standardise the compliance framework. In fairness, NHS Digital have made a great start already.
A typical day for you would include…
Well, like most innovators I still have another job. I am a full time clinician, so I guess a busy shift in resus dealing with major trauma and sorting out sick patients. The meetings, writing documents, talking to the developers, managers, IT people and interested parties all happen around my clinical commitments. I wouldn’t have it any other way as this keeps it real.