Londoners have set out how they expect their health and care data to be used, as part of a London-wide Citizens’ Summit. There was strong endorsement for joining-up information held by the NHS and care services to improve care for individuals and for the population, as long as certain conditions are in place.
In receiving these detailed recommendations, local health and care leaders confirmed that these public expectations will be used to shape policy for London, ensuring that Londoners can have confidence in how their health and care data is used.
The OneLondon Citizens’ Summit was a large scale and in-depth public deliberation on uses of health and care data. It involved 100 Londoners in a four-day process of detailed discussion and debate. Participants reflected London’s diverse population, came from all 32 boroughs, and had a mix of attitudes towards data sharing. They were provided with technical information by experts and practitioners. The work was overseen by an independent advisory group.
This Citizens’ Summit is a new and innovative way to involve the public in policymaking. As a result, Londoners have had more opportunity than ever before to be informed about the issues and trade-offs, and to set out their expectations about the uses of their health and care information by the health and care system.
The Citizens’ Summit was commissioned by London’s five health and care partnerships via the OneLondon Local Health and Care Record Exemplar (LHCRE) programme, and delivered by Ipsos MORI and The King’s Fund. Through public deliberation, London is leading the way in understanding how citizens weigh-up the benefits and potential concerns of data use, to reach an informed set of public expectations that will now shape the development of policy across the capital.
How do Londoners expect their health and care data to be used?
• Access and control in health and care data
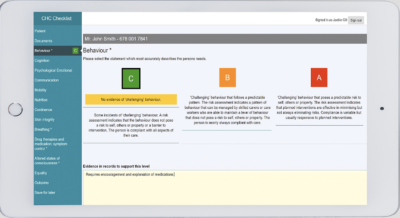
At the end of the process, after four days of deliberation, there was almost unanimous agreement (97 per cent of those who attended on the day)* that all health and care organisations in London should join up identifiable data to support the provision of care to individuals. An expectation was set that health and care professionals would only have access to information relevant to their roles through a means of role-based access control. Strict conditions were set out by Summit participants, taking into account the level of urgency of a patient’s condition, safeguarding of information and accountability.
• Use of de-personalised data for health and care planning and improvement
Participants recommended that de-personalised data must be used by relevant organisations to plan and improve services and demonstrably benefit the health of the population, with conditions set out to ensure security of data, transparency of access, and an individual’s choice to opt out of this use if they wish.
• Use of de-personalised data for research and development
Conditions for using de-personalised data to support research and development included who should have access (including commercial organisations) and how they should be charged for this access, with a tiered pricing model being suggested. Participants also set conditions around how information should be safeguarded and accessed in a safe and secure setting, and how benefits – financial and otherwise – should be realised and distributed across the NHS.
• Governance and oversight
There was a strong expectation set that citizens are involved in ongoing policy and decision-making around the uses of health and care data as part of a continuing diverse citizens’ advisory group, with a request for those in elected positions, for example, the London Assembly, to play an oversight and scrutiny role.
• Consistency across London
After four days of deliberation, nearly all of the participants (98 per cent of those who attended on the day)* stated an expectation that all health and care organisations in London must join up de-personalised information, as part of a population dataset, to support proactive care, planning, improvement, research and development in line with the recommendations and conditions they set out.
What does this mean for London’s health and care system?
Data collected about a person’s health and care offers a range of benefits – from helping NHS and care staff to provide safe, quality care, to planning and improving services, to supporting research and discovery of new treatments. The public health emergency of the Covid-19 pandemic has highlighted more than ever the need for a joined-up approach in using data, both now and into the future. This is an expectation shared by Londoners, and the recommendations formed by participants through the Citizens’ Summit provide a clear directive to the health and care system.
One participant involved in the Citizens’ Summit, said:
“I consider my healthcare information to be very personal and it’s important that it is discussed openly as to whether we want that to be shared, or the extent to which it’s shared. It’s very democratic to be part of this process. We can often feel, politically, quite impotent as individuals, so being able to feel like the opinions I’m expressing are going to be helping to shape policy… it’s really good to be a part of it.”
A second participant commented:
“Certain expectations that I had of the NHS and our data were completely blown out of the park. Connections I thought might be there – or hoped were there – weren’t. So it’s been very informative. I came in initially with the view that, ‘the data is mine, no one should have access to it’, so I’ve done a big flip. It’s been a journey because I’ve kept flipping to and fro.”
Dr Vin Diwakar, Regional Medical Director for the NHS in London, commented:
“Having listened to Londoners about how they expect their personal health information to be used, it is clear they want those treating patients to have access to all the health and care information for those individuals, to optimise care. They also strongly support using data for research and the clear benefit of improving the city’s health and social care. Privacy and other safeguards must be in place. We are grateful for the involvement of all those who took part and will continue to work closely with Londoners as we look to develop an agreed set of principles for how we safely and securely use Londoners’ data, based on their recommendations.”
London’s Chief Digital Officer, Theo Blackwell, said:
“There is huge potential to harness health and care data in a safe and secure way, in order to improve Londoners’ wellbeing while protecting their privacy. The Mayor and I are clear that Londoners must be at the heart of shaping how their data is used and by whom. The OneLondon Citizens’ Summit has empowered Londoners to make recommendations on this important issue, to ensure the system can develop policy in a trustworthy way.”
Recommendations and findings from the OneLondon Citizens’ Summit are detailed in a new report. Download Public deliberation in the use of health and care data here.
For more information visit One London website.
“Having listened to Londoners about how they expect their personal health information to be used, it is clear they want those treating patients to have access to all the health and care information for those individuals, to optimise care. “Dr Vin Diwakar, Regional Medical Director for the NHS in London