What are the benefits of advance care planning using digital tools and how challenging is it to implement an effective system? In this Q&A discussion, NHS South West London CCGs Digital Urgent Care Planning Project Officer Lucy Colleer and NHS England Assistant Director for Enhanced Health and Care Homes and Care Sector Support Fay Sibley answer key questions in the aftermath of Covid-19 and its impact in care homes. The conversation centres on the advance digital care record, Coordinate My Care (CMC).

Photo above: Fay Sibley
Why is advance care planning and having a digital urgent care record important for care home residents?
Fay:
I think it's incredibly important that care home residents have a digital urgent care record. We know that care home residents are often in the end phases of life. Even those that aren’t, are living with often extremely complex health and social care needs. So to have a single place where information is recorded about their wishes and preferences as well as their medical needs, including their medication, diagnosis and CPR status means that we are able to look after care home residents in a more holistic way.
"I think that's particularly important when we start to think about people who, for various reasons, aren’t able to necessarily advocate for themselves."Fay Sibley
It means that all of the health care professionals who are involved in that person’s care, and look after that person have access to information about that person. I think that's particularly important when we start to think about people who, for various reasons, aren’t able to necessarily advocate for themselves. Or may not be well enough at the point in which they're accessing care to be able to advocate for themselves, or to put forward their needs and preferences.
Putting in place a system
To have that in a systematic way that's consistent and that everybody is familiar with, really does help them with transfer of care. This means we can make sure that we do meet those wishes and preferences and just means we can deliver the right care. Whether that's keeping somebody comfortable at home, or whether that's escalating and transferring them to hospital. If you can access that information, it allows you to consider that on a very individual basis.

Bitesize info
A series of short case study videos have been produced to demonstrate the value of individual patients having advance/urgent care plans brings to the wider health and care system.
Photo above: Lucy Colleer
Lucy:
We conducted a case study recently with a care home in Kingston, to look at how they were using CMC. How they got on with setting up CMC in the care home as well as getting their staff trained and using it. I think the biggest benefit, is that [CMC] puts the resident’s wishes first.
From a technical point of view, having a digital urgent care plan allows everyone to have access to the same information. It’s updated automatically, which means that you don't have to worry about bits of paper going out of date or going missing.
Saving time in an urgent situation
One of the things that the care manager we interviewed spoke about, was that it saved them so much time in an urgent care situation. In one instance, they had a resident who had a fall, and they called the ambulance service. Normally they would get phone calls from A&E saying, ‘What are the patient’s medical details?’, ‘What medication are they taking?’ But having it in that digital care record just meant that they didn't have to spend time printing documents, or taking those phone calls. And also for the staff in A&E as well, it was really helpful to have that information. Having an End of Life care plan really saves time and can strengthen decision-making.
It's just about putting the resident and the patient first. It also helps make life easier for clinicians who don't have an awful lot of time on their hands, and the care home staff as well.
"(A CMC care plan) really means that we are able to look after care home residents in a more holistic way."Lucy Colleer
Bitesize info
In July 2020, the HIN was commissioned to deliver a programme to increase use and quality of shared electronic advance and urgent care plans using Co-ordinate my Care (CMC). The programme concentrated on clinical engagement. Read about the Advance and Urgent Care Plans – London Accelerator
Fay:
I used to work for the ambulance service and one of the most difficult things was going to a care home in the early hours of the morning after being called to a resident. In one instance where this happened to me, the resident was acutely unwell, had a complex medical history and wasn't able to communicate. I was faced with trying to make an informed clinical decision with no access to information. Often at night in a care home they're operating with skeleton staff and, quite often, agency staff or bank staff because there are challenges in the care sector workforce. So they might not even be able to access patients records because they would be locked in the manager's office.
The problem with limited information
What we would know about that resident would be so limited that often as a paramedic, you end up taking people to A&E despite having concerns about whether the distress that course of action entails would justify the benefits. At that point it comes down to questions around what is “right” or “fair”, which are very difficult to answer as a clinician.
You are so limited to be able to make any other choice, because you didn't know their medical history. You didn't know what their wishes were. Nor which family member to call or who might have some more information about that person.
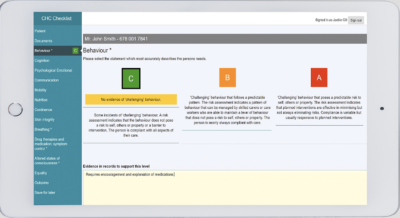
Seeing the info on an iPad
When paramedics first started to be able to access urgent care records we used to have to do that by phoning up the control centre. Amazingly, now paramedics can actually see it in real time on an iPad. But even when I left the service, you could call up the control centre and ask for that information. It just meant that you could make a different decision and you could justify that decision.
It was an informed clinical decision that was backed up and supported by the input of that person's GP. The input of that person's family, the input, hopefully, of that person themselves, as it allows you to make different decisions. And as Lucy said, a decision that really puts the person at the centre.
"There was real recognition that care needed to change quite quickly [because of Covid], and that those effects would probably be lasting."Fay Sibley
Bitesize info
The HIN, in partnership with the End of Life Care Strategic Clinical Network, secured funding from the NHS England (NHSE) personalisation team to work with Marie Curie nurses to create CMC records for care home residents in three nursing homes in south east London over a five week period. Read Increasing the number of care home residents in Lambeth supported by a Co-ordinate My Care plan
How is the HIN doing in terms of speeding up the spread and adoption of digital urgent care records in south London?
Fay:
The HIN has been working in this space for a long time, probably since the HIN started (in 2016) and more formally with CMC for the last two and a half years. Through a small pot of funding, through The Health Foundation, we were able to do a pilot project with about 10 care homes looking at different methods of getting care homes access to CMC. We also looked at the things that care homes would need to do in order to be able to access CMC. Either to view it or to put information into the record.
The challenges for care homes
From that project we learnt an awful lot about some of the process aspects of this that are challenging for care homes. Things like Information Governance (IG) requirements, the hardware requirements, having a laptop or a device to use and the Wi-Fi requirements. I think that learning has then helped us to try to move this conversation on.
Obviously in terms of the [Covid-19] pandemic, it changed lots of things. Particularly the work that care homes are doing and the focus being put on care homes by the Government. So at the beginning of the pandemic the HIN was really instrumental in trying to pull together various stakeholders who were looking at the key questions ‘How do we create records for care home residents?’ There was real recognition that care needed to change quite quickly, and that those effects would probably be lasting.
Collaborative working
The other thing we did was we worked with the End of Life Care Strategic Clinical Network to secure some funding and ran a small-scale pilot with Marie Curie. That was really interesting because Marie Curie had a number of frontline clinical staff who were shielding themselves because of the pandemic. Those staff were at risk of being furloughed and not able to work because they weren't able to do their frontline job. So what Marie Curie did was give them some additional training and upskilling. This meant they could support care homes to create CMC records for residents.
Working with care homes
We worked with three care homes in Lambeth, one GP practice and Marie Curie to deliver a small kind of, ‘proof of concept’ project around the use of CMC in a care home. We learnt lots. We realised that to create quality records remotely with another organisation that doesn't perhaps know that person or have access to all of their clinical information has its challenges. They were able to do a fantastic job in starting the record off, but they still required a fair amount of input from the GP. It was not a perfect model, but we learnt a lot from the project. It was really interesting to use voluntary sector organisations to support this work. In particular, organisations like Marie Curie that really have a lot of knowledge around end of life and advance care planning. And to use a staff group that otherwise, perhaps, wouldn't have been working during the pandemic and certainly couldn't do their main role.
Bitesize info
The HIN Healthy Ageing and Informatics Teams were commissioned to create a user friendly and useful digital maturity dashboard for care homes across London. This project was led by the Health Innovation Network and funded by the Digital First London region team.
Since then we've been doing a lot of work with Lucy and trying to support the coordinated pan-London effort around care homes and CMC. So it's absolutely brilliant to see this is on the commissioners’ radar and the work that Lucy’s doing. Lucy's pulled together a steering group that now meets monthly, and the HIN is also trying to help with some of the analysis of the data.
A dashboard for care home digital maturity
We've developed a Care Homes Digital Maturity Dashboard. This is a tool to be able to monitor each care homes maturity status, in terms of their digital abilities. A key part of that for London care homes is CMC. 'Do they have access to CMC?' 'Do they have the right IG requirements that allow access to CMC? 'How many residents in their home have CMC?' We’re pulling all of those data sources together and presenting that information in a way that's useful to Lucy and other colleagues across London working in this space.
I think the HIN’s moved more into a supportive role, trying to share the lessons that we've learned from some of the early work. And then really letting the commissioner drive it forward in a way that we don’t have the reach to do.
"(A CMC care plan) really means that we are able to look after care home residents in a more holistic way."Lucy Colleer
Bitesize info
View the collection of resources. Coordinate My Care has provided a wealth of info to support the patient-led portal to create an end of life care plan. MyCMC: your plan, in your own time, in your own home
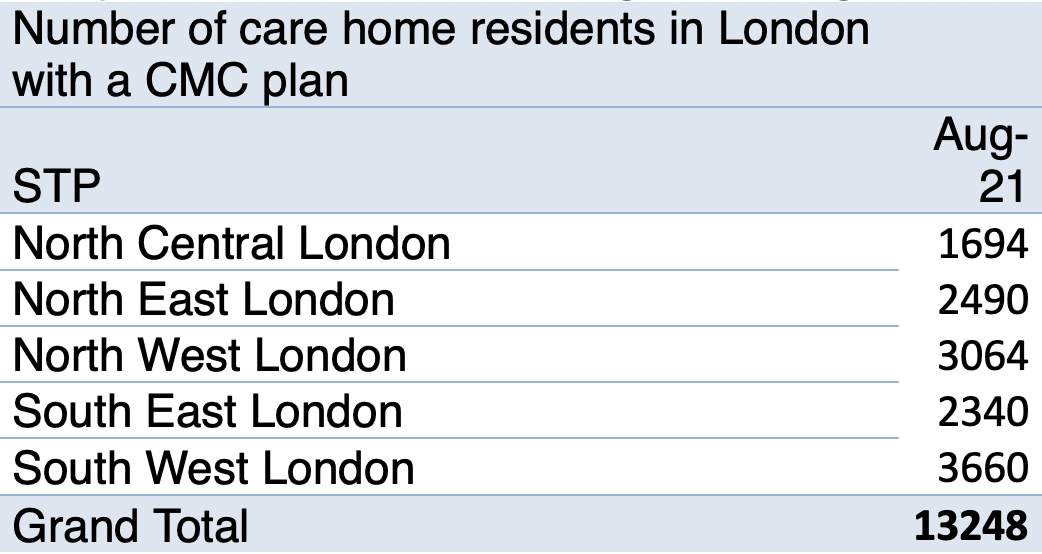
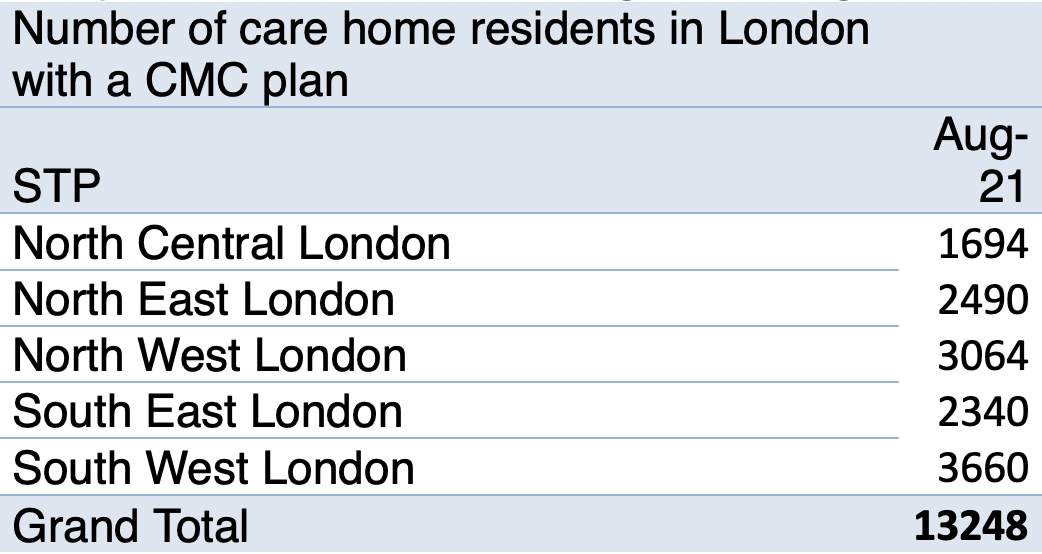
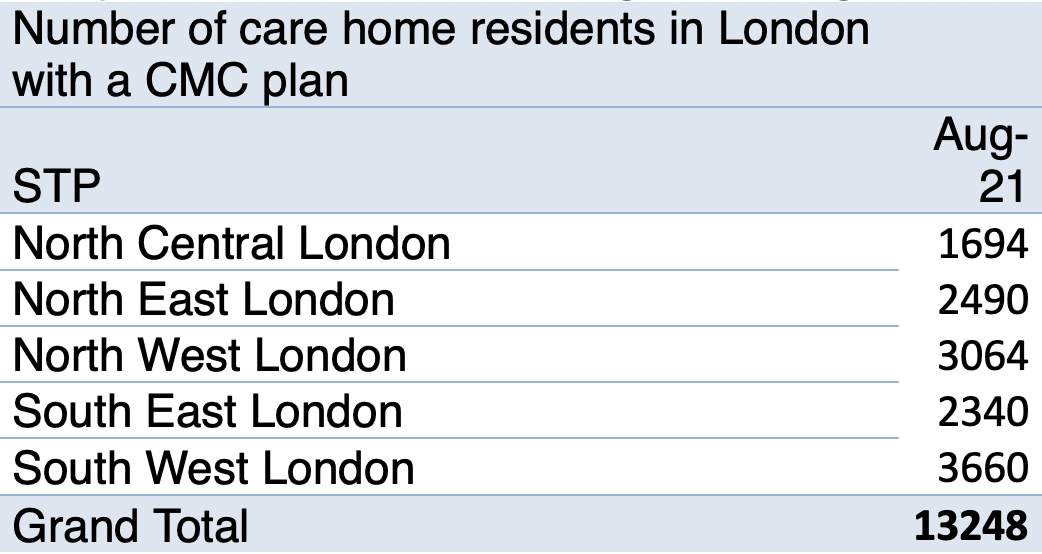
How many digital urgent care records have been created through CMC?
Lucy:
It’s in the region of thousands (see chart below). There are lots and lots of residents who do have care records, so the focus of our pan London work at the moment is actually getting care home staff themselves to look at those records. At the moment the majority of those records are created by the GPs and sometimes in the acute trust. So we're trying to encourage care home staff to start looking at those resident plans and keep them up to date.
The power of data
We have been working really closely with Fay and the HIN and I would say that the HIN has been more than just support. We're trying to lead the way from where you paved the way and the Care Homes Digital Maturity Dashboard is really, really helpful especially from a commissioning perspective because we can look at how it's affecting the ambulance call-outs and the conveyance rates and use the information to make commissioning and transformation decisions. From a commissioning point of view, obviously patient-centred care is the most important thing, but financial return on investment is important too. It’s been really great to be working with it with the HIN and supporting work that Fay and the team have been doing.
Fay:
I think the other thing that's really helpful is about data, and CMC actually produce a fair bit of data. Again we could debate the data set of course we could, but they do produce a commissioners’ workbook, again on a monthly basis. One of the useful things about data is it allows you to look at different areas and make those comparisons.
Incentivising GPs and the role of the ICS's
For example in south London, south west London do particularly well in terms of the number of CMC records they’ve created. So you can look at some of the models that they've put in place over the last, let's say five years, that have really led to that. For example they incentivised GPs to do some of this work, so you saw a really big increase in that they've got a really established enhanced health and care homes programme and End of Life care programme within their Integrated Care System (ICS).
Again, they're really driving that work forward from a ICS strategic point of view, so having data allows you to look at factors such as where’s doing well? And ask questions like 'What are they doing?' 'Who’s lagging behind and 'what might be the reasons for that?'
The quality of the record
And then one of the other things that the HIN has really been focusing on is thinking about the quality of the record. Creating a record is one thing that's really important, but the record is only really as good as the information that's in it. 'How do I make sure that the information that I include in that record is of quality and is useful?' 'Does it make sense as a kind of complete picture?'
The HIN developed a checklist of the non-mandatory information that would be most useful to clinicians. And then from that we've done some work with south west London to try to refine that. Again, we pulled together a steering group with various clinicians from south west London to look at how can we use something like a checklist to drive up and standardise the quality of CMC records. This is so they are a useful, high quality, advanced care planning record.
"Creating a record is one thing that's really important, but the record is only really as good as the information that's in it."Fay Sibley
What would you say has been the biggest challenge in setting up more CMC records?
Fay:
I think capacity of the workforce to really do this, is the biggest challenge. As Lucy said, at the moment the vast majority of CMC records for care home residents are created by GPs. But GPs are an incredibly over-stretched workforce and it's not a quick five-minute job. It can take up to an hour to really have a meaningful conversation and then translate that into a record and publish that record. When you start talking about thousands of records across London, that's thousands of hours of GP time.
Who else can support the programme?
But I think the thing that may help us around that is understanding who else within the primary care and community services workforce can support this work. Care homes themselves absolutely play a vital role and can feed into the record and do some of the data entry and have the conversations, but also, say, palliative care teams often do this kind of work; hospices, they've got brilliant teams that can support with this. Voluntary sector organisations; Macmillan, Marie Curie and GP practices are now starting to grow their workforce. Through the Primary Care Networks, we've now got paramedics working in GP practices. We've got highly skilled nurses that are really, really knowledgeable. There is a growing pool of professionals who could support the creation of urgent care records.
Getting patients and their families involved
We’ve also got an opportunity through MyCMC potentially as well which is something that was set up to be a patient-led record. Somebody would initiate that record for themselves, and there are roles within a GP practice where that could be a supported process, so social prescribers for example have the potential to be able to support somebody, even living in a care home, to initiate that record. People have a bit more agency. This includes setting up a record in mental health care homes and learning difficulty care homes. It may be appropriate sometimes to use MyCMC.
Lucy:
I take your point on capacity in terms of creating and maintaining those care plans. Once the plan is there, it’s fairly easy to update and maintain it and we've seen that with some of the care homes that have been using it. They include it as part of the weekly rounds when the GP comes along, they include it at the Multi-Disciplinary Team (MDT) meetings that take place. And actually it's not too much work once the initial plan is filled out. In some of the more successful care homes using CMC the biggest thing, is just being engaging with them, and that's quite difficult to do from a commissioning perspective.
Resource challenges
I work in a very small commissioning team of just two. We’re covering the whole of London, including all health and care organisations across London. So between us, it's very difficult to do that engagement. CMC does have a very strong engagement team, and they are successful, but they're still quite a small team for the whole of London. Some of the more successful care homes have been the ones that the CCG has provided resource, such as project support officers that have literally been hand holding those care homes to support them with all sorts of digital maturity aspects, like the Data Security and Protection Toolkit (DSPT) compliance and also, they've been really helpful with getting the care homes access to CMC.
I think engagement is one of the biggest success factors, but also a huge challenge. I think there's such a variety of resources across London. I know some STP's simply just don't have the resource to hand hold care homes with it.
Care homes 'left behind'
I think care homes have been left behind a little bit in terms of digital maturity. That's one of the key things - being able to have access to a computer, good internet, the IG (Information Governance) - all in place. I think that they've been a bit left behind. I don't know what the historical reasons behind that are, but I think the digital maturity side of things is a big challenge for some care homes, especially the smaller ones.
Fay:
I would agree wholeheartedly with that around the kind of digital maturity aspects.
And I think there's lots of reasons. Obviously, many of them are private providers. Historically, social care hasn't received the same level of funding as the NHS. It perhaps hasn't been seen as a priority or our job.
Equality of access to care
But I think when we talk about and think about equality of access to care and the world that we now live in, and the fact that many health services have been forced to, at least in some ways, move to a more virtual remote delivery then actually it's no longer the responsibility of social care alone because we're denying people access to the care that they have a right to.
I think that's probably why there is such an increased focus throughout the pandemic on getting care homes up to that basic level of digital maturity; that same digital standard that we would expect of our NHS. It's not easy, and I think one of the reasons we started the dashboard was because at the beginning of the pandemic, what we didn't know is what we didn't know (i.e we didn't know whether this home in Southwark had Wi-Fi even, or if they even had a laptop and that information wasn't anywhere). There were no agreed datasets around the care homes. There was no kind of central repository to go to and just put in the care home name and it will bring that up, so we didn't even know how to support them, because we didn't know what they had to start with. So that's part of the reason we initiated that dashboard work because we were like how we can support the central government functions - health and social care, public health and other involved organisations?
This was a joint interview that took place remotely in April 2021.
NB: Fay Sibley was speaking in her previous role as the HIN's Head of Healthy Ageing.
Explore our website for more
See more info on our work with CMC here.
Click here for the CMC project webpage