As part of Type 2 Diabetes Prevention Week, Faye Edwards, Senior Programme Manager for diabetes at the HIN, writes about the HIN-backed services which are helping improve access to essential support for people living with diabetes.
For those working in the NHS, particularly primary care, the ever-increasing number of people diagnosed with type 2 diabetes can feel like an uphill climb that just keeps getting higher. Across south London around 180,000 people are living with diabetes, over 120,000 have non-diabetic hyperglycaemia (pre-diabetes), and many more people are undiagnosed.
"For those newly diagnosed with diabetes it can feel overwhelming, confusing and even isolating."
For those newly diagnosed with diabetes it can feel overwhelming, confusing and even isolating. As with any new diagnosis it can take a while for people to understand the implications, and how they should manage their future health. Diabetes education and personalised, supported self-management are vital in the prevention and long-term management of type 2 diabetes, which is why they are priorities for the NHS.
The Health Innovation Network has had a focus on diabetes since 2014 and during our work with local people the importance of access to diabetes education and peer support became really clear. In 2017 the HIN convened the 12 south London clinical commissioning groups to collaborate and create Diabetes Book & Learn, a service to help people access diabetes education wherever they choose in south London. This cross-boundary working is a great example of how commissioning can enhance patient care and deliver a wide choice of options, achieving an economy of scale that would be impossible to deliver alone.
Across south London the Diabetes Book & Learn service provides people with type 2 diabetes with a wealth of education options, including group sessions led by a specialist diabetes dietician or nurse, delivered in person or online, depending on individual preference. These group courses include the DESMOND and X-PERT HEALTH programmes, both of which are well established, quality assured type 2 diabetes education programmes delivered by trained educators. It also includes HEAL-D, which is a culturally-tailored type 2 diabetes education course for people of African or Caribbean heritage, created in partnership with members of the African and Caribbean communities in south London.
Book & Learn Digital also has a range of options that provide diabetes education and self-management support via a mobile app or telephone. These include the Low Carb Program, which provides structured education, coaching and support on how to self-manage your type 2 diabetes and uses AI to provide personalised recipe and exercise suggestions; and Second Nature, which uses behavioural insights to support people with type 2 diabetes to make lifestyle changes and gain knowledge of self-managing the condition.




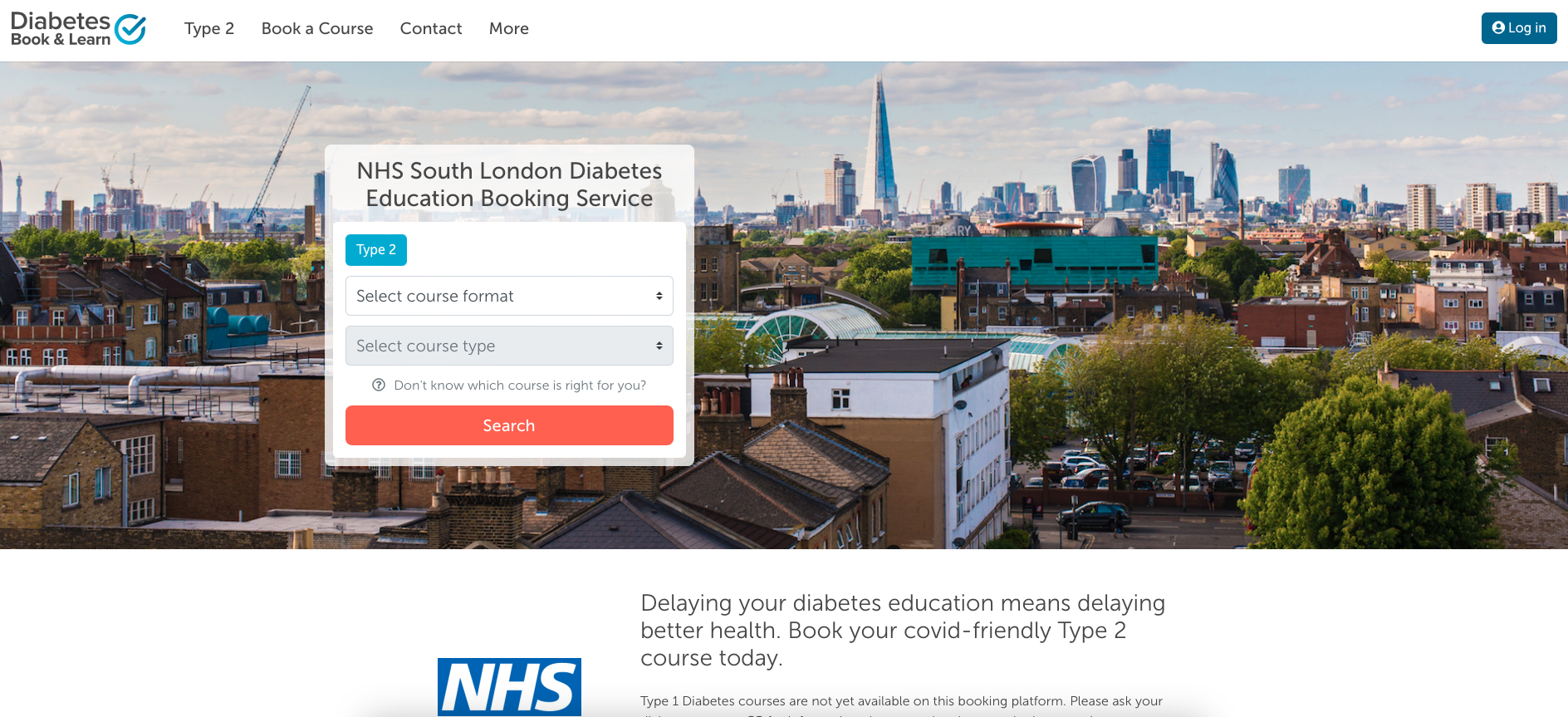
Since the launch of Diabetes Book & Learn in 2018 the we have continued to support its development. During the pandemic we support the ICBs with the procurement of new digital services and facilitated the switch of in-person sessions to online delivery, keeping the service going when many other similar services in the NHS had been temporarily stood down. Since Diabetes Book & Learn began, over 14,000 people with type 2 diabetes have been booked into a diabetes education course, with over half of these people choosing our digital or online options.
The establishment of Diabetes Book & Learn at scale across south London provides an unrivalled choice of education options for people with type 2 diabetes. It is playing a vital role in simplifying access to key self-management support and encouragement, and is equipping people with type 2 diabetes to take control of their future health and wellbeing. No one with a diagnosis of type 2 diabetes in south London should feel overwhelmed, confused or isolated by their diagnosis: Diabetes Book & Learn is here to help.
Find out more
People with type 2 diabetes who are registered with a south London GP practice can self-refer at the link below or call our friendly call centre team on 020 3474 5500. Any health care professional can make a referral via our website, call centre or via their practice IT system.
Diabetes Book & Learn