Our Mindset-XR Innovation Support Programme spotlight for October is on Greener Games - a UK-based immersive health company specialising in extended-reality (XR) experiences that support emotional wellbeing and mental health. Building on the international success of Nature Treks VR, used by over 300,000 people worldwide. Greener Games is now developing Harmony, a personalised XR platform that helps people explore, express, and regulate emotions in safe, nature-inspired environments.
Currently in collaboration with Greater Manchester Mental Health NHS Foundation Trust, Harmony is being designed for use with people experiencing moderate to severe mental-health conditions, with the long-term aim of rolling it out to multiple NHS Trusts across the UK.
Below, we hear from co-founder Ria Kalograni, who shares insights about the company and its innovative approach to wellbeing.
How has user feedback shaped your product?
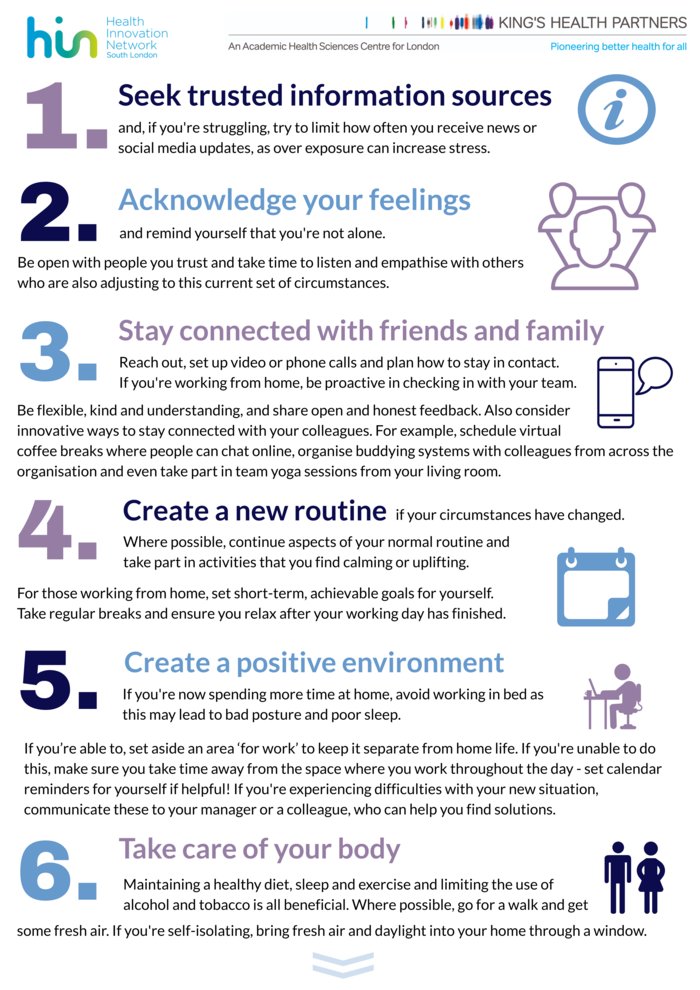
Feedback from a wide range of settings, including NHS clinicians and patients, has influenced the development of Harmony, from the pacing of sessions and sensory balance to the accessibility interface.
Their guidance ensures Harmony feels safe, intuitive, and genuinely therapeutic for people managing anxiety, trauma, or depression.
What is the biggest challenge you have faced so far in developing your innovation?
Our main challenge has been aligning immersive technology with clinical frameworks and NHS digital standards.
Balancing creativity with compliance requires time, patience and precision, but with early feedback from NHS Manchester and support from Mindset XR, we are building strong foundations for the future.
Why should the health and care system be excited about your innovation?
Harmony combines nature, neuroscience, and therapy to offer a safe, evidence informed way to support mental health. It helps clinicians extend care beyond traditional settings, reaching people wherever they are.
By bridging socioeconomic and accessibility gaps, Harmony opens the door to healing, calm and connection for those who might otherwise be left behind.
What XR success stories would you like to share with us?
A very proud moment was seeing Nature Treks VR featured by the BBC in an NHS setting, supporting women through miscarriage by helping to reduce trauma and anxiety.
It is a deeply moving example of how immersive environments can bring comfort and calm when it is needed most.
bbc.co.uk/news/health-60941650
What type of support are you seeking most from readers to help drive your project forward?
We are looking to connect with more NHS Trusts interested in exploring how Harmony can enhance wellbeing and therapy delivery.
We also welcome partnerships that can guide our digital-health accreditation, evaluation, and procurement pathways, any educational setting in helping us bring Harmony into wider use as an accessible tool for support and recovery.
Founded by John Carline and Eleftheria (Ria) Kalograni, Greener Games creates immersive experiences that nurture calm, connection, and creativity. Their mission is to harness technology not as an escape from the world but as a bridge back to nature, self-awareness, and healing.
ekalograni@greenergames.net
Want to find out more about our Mindset-XR Innovation Support Programme?
Sign up to our monthly newsletter and keep up to date with all the latest news
Click here